LEONARDO F. L. RIZZO1, DANIELA L. MANA1, HÉCTOR A. SERRA1, 2
1Dirección Médica Química Montpellier SA, 2Cátedra de Farmacología, Facultad de Ciencias Médicas,
U.C.A., Buenos Aires, Argentina
Abstract The thyroid axis is particularly prone to interactions with a wide variety of drugs, whose list increases year by year. Hypothyroidism is the most frequent consequence of drug-induced thyroid dysfunction. The main mechanisms involved in the development of primary hypothyroidism are: inhibition of the synthesis and/or release of thyroid hormones, immune mechanisms related to the use of interferon and other cytokines, and the induction of thyroiditis associated with the use of tyrosine kinase inhibitors and drugs blocking the receptors for vascular endothelial growth factor. Central hypothyroidism may be induced by inhibition of thyroid-stimulating hormone (bexarotene or corticosteroids) or by immunological mechanisms (anti-CTLA4 or anti-PD-1 antibody drugs). It is also important to recognize those drugs that generate hypothyroidism by interaction in its treatment, either by reducing the absorption or by altering the transport and metabolism of levothyroxine. Thus, it is strongly recommended to evaluate thyroid function prior to the prescription of medications such as amiodarone, lithium, or interferon, and the new biological therapies that show important interaction with thyroid and endocrine function in general.
Key words: thyroid, hypothyroidism, drugs
Resumen Hipotiroidismo inducido por drogas. El eje tiroideo es particularmente proclive a sufrir interacciones con una amplia variedad de drogas, cuya lista se acrecienta año a año. El hipotiroidismo es la consecuencia más frecuente de disfunción tiroidea inducida por fármacos. Los principales mecanismos involucrados en el desarrollo de hipotiroidismo primario son: la inhibición de la síntesis y/o liberación de las hormonas tiroideas, mecanismos inmunes relacionados con el uso de interferón y otras citoquinas, y la inducción de tiroiditis asociada al uso de los inhibidores tirosina-kinasa y a drogas bloqueantes del receptor del factor de crecimiento del endotelio vascular. El hipotiroidismo central puede ser inducido por la inhibición de la tirotrofina (bexaroteno o corticoides) o por mecanismos inmunológicos (drogas anti-CTLA4 o anti PD-1). Es importante reconocer aquellas drogas que generan hipotiroidismo por interacción en su tratamiento, ya sea disminuyendo la absorción o alterando el transporte y metabolismo de la levotiroxina. Sería recomendable evaluar la función tiroidea previa a la prescripción de medicamentos como amiodarona, litio o interferón, y a las nuevas terapias biológicas que muestran importante interacción sobre la función tiroidea y endocrina en general.
Palabras clave: tiroides, hipotiroidismo, fármacos
Received: 21-VII-2017 Accepted:15-IX-2017
Postal address: Dra. Daniela Mana, Maza 578, 1220 Buenos Aires, Argentina
e-mail: daniela.mana@gmail.com
The thyroid axis is particularly prone to interactions with a wide variety of drugs and natural substances, the number of which increases every year. These substances affect every aspect of thyroid physiology and hormone pharmacology1. It is therefore important to recognize these interactions in order to avoid therapeutic failures, unnecessary therapies or false diagnoses2. These interactions lead to different forms of thyroid disorders (dysfunction, goiter, etc.), the most common of which, hypothyroidism2, will be discussed below.
The mechanisms responsible for drug-induced hypothyroidism can be summarized as follows2:
a) Inhibition of synthesis and/or release of thyroid hormones
b) Immune mechanisms
c) Drug-induced thyroiditis
d) Mixed: tyrosine kinase inhibitors
e) Inhibition of tyroid-stumulating hormone (TSH) synthesis
f) Interactions in the treatment of hypothyroidism
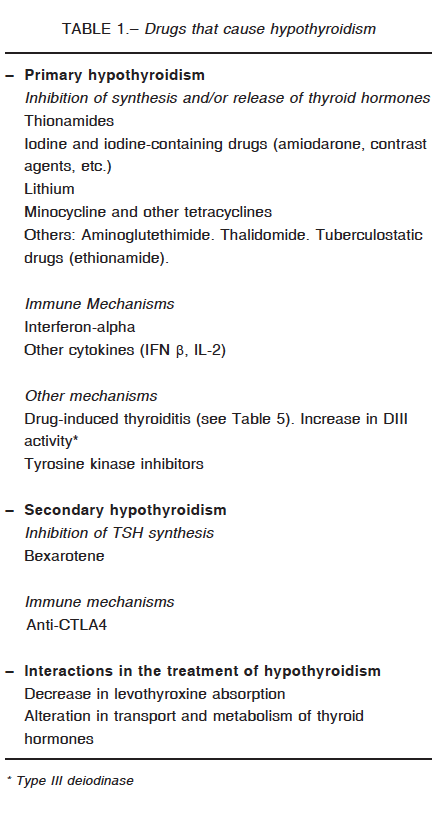
Many drugs can induce both primary and central hypothyroidism through different mechanisms. Table 1 displays a list of these drugs and mechanisms.
Drug-induced primary hypothyroidism
a) Inhibition of synthesis and/or release of thyroid hormones
1. Thionamides
Their inhibitory effect on thyroid function has been known since 1943. Astwood suggested the use of thionamides to treat hyperthyroidism and named them antithyroid drugs3. Their main action is to interfere with thyroid peroxidase both in the oxidation and organification of iodide and in the iodotyrosine coupling process4. Since antithyroid drugs are used to treat hyperthyroidism, their pharmacological effects should not be considered undesirable.
2. Iodine and iodine-containing drugs
Iodine was discovered in 1811 by Bernard Courtois and its name comes from the Greek word “iodes”, which means violet5. The main effects of iodine excess on the thyroid are6, 7:
– Decrease in iodide transport
– Decrease in iodide oxidation and organification (Wolff-Chaikoff effect)
– Rapid blockade of thyroid hormones release through inhibition of intrathyroidal lysosomal activity, preventing thyroglobulin hydrolysis
– Immunostimulation
– Decrease in thyroid vascularization
An excessive iodine intake increases the risk of hypothyroidism and thyroid autoimmunity7. The thyroid cell has several self-regulating functions protecting it from a sudden increase in iodide serum levels. In the presence of high concentrations, there is a decrease in iodide oxidation and thyroid hormone synthesis (Wolff-Chaikoff effect). This effect is usually transient in normal individuals, an “escape” phenomenon occurring in approximately two weeks. The efficiency of the sodium/iodide symporter decreases over a few weeks, thus restoring the intrathyroidal iodide pool and thyroid hormone synthesis toward normal8.
In normal individuals, exposure to pharmacological doses of iodine normally produces a slight temporary decrease in thyroid hormone levels. In patients with lower thyroid reserve (autoimmune thyroiditis, goiter), the escape from the Wolff-Chaikoff effect is impaired, resulting in hypothyroidism6.
The predisposing factors for Iodine-induced hypothyroidism are8:
– Autoimmune thyroiditis
– Post-treatment of hyperthyroidism
– Previous hemithyroidectomy for the treatment of nodular goiter
– A history of postpartum thyroiditis, subacute thyroiditis, drug-induced thyroiditis
– Thalassemia major (thyroid hemosiderosis)
– Chronic renal disease
In euthyroid patients (especially children and the elderly), acute exposure (computed tomography scan with contrast agent)9 or prolonged exposure (topical or systemic) to iodine may result in hypothyroidism which is resolved by withdrawal. As iodine easily passes through the placenta, it can induce fetal goiter or hypothyroidism. Vaginal application of povidone-iodine during delivery, or topical use of disinfectants in newborns may also promote transient neonatal hypothyroidism10.
Exposure to iodine-based compounds is also reflected in alterations of laboratory tests11:
– TSH increase
– Decrease in thyroid hormones levels
– Increase in the amount of urinary iodine excretion over 24 hours
Even the administration of kelp-based preparations may affect thyroid economy modifying the hormone profile11.These alterations return to normal within 2-3 weeks following treatment withdrawal, with the exception of contrast agents and amiodarone (see below).
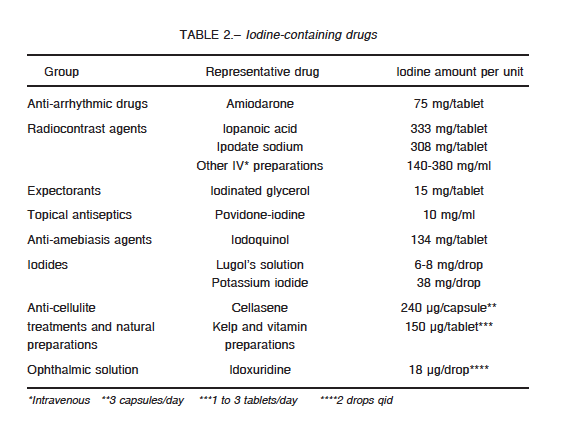
The main iodine-containing drugs are shown in Table 2.
Iodinated contrast agents
They are used in a wide range of imaging studies, such as angiography, venography, pyelography, endoscopic retrograde cholangiopancreatography, myelography and computed tomography scan among others.
Hydrosoluble preparations used in diagnosis and angioplasty contain 30-60% of iodine. In general, 70-100 ml are used per study (which provides 30-35% of the halogen).
Around 20% of patients (without previous thyroid pathology) may develop thyroid dysfunction (hypo and hyperthyroidism) following administration of an iodinated contrast agent9.
In patients undergoing contrast studies, it is advisable to wait for two months before administering radioiodine (diagnostic or therapeutic). It is advisable to rule out thyroid pathology before indicating contrast studies, especially in children, elderly patients and patients with renal insufficiency9, 12.
Amiodarone
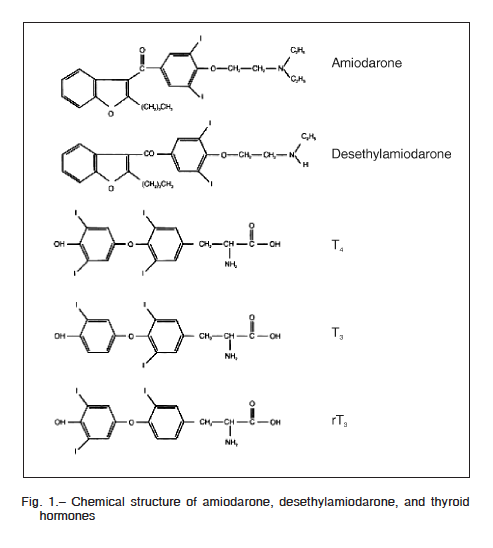
Amiodarone is a benzofuran derivative with high iodine content (39% of its molecular weight). There is a structural similarity between amiodarone, its main metabolite: desethylamiodarone (DEA), and the thyroid hormones (Figu-re 1), so the drug behaves as a partial agonist of these hormones developing agonist activity in tissues such as the pituitary gland and antagonist activity in the heart13, 14.
Each 200 mg tablet of amiodarone contains around 75 mg of iodine, so a 200-600 mg/day dose releases 7-21 mg of inorganic iodine into the systemic circulation during its hepatic metabolism14. This represents a contribution 50-100 times higher than the recommended daily intake of iodine of 150-250 μg. Deposits of the drug will be found in the adipose tissue, the liver, the connective tissue, the heart and the skeletal muscle, and the thyroid gland itself. It has an elimination half-life of around 100 days15. Amiodarone clearance is reduced in obesity by 22% and in patients over 65 years of age by 46%16. Due to its extensive tissue accumulation, the drug’s effect persists between months and years after withdrawal.
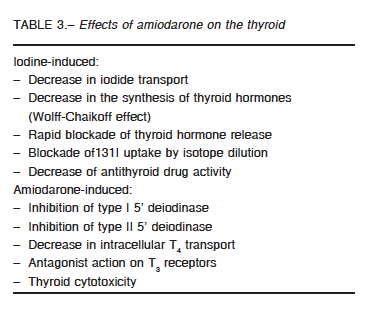
The effects of amiodarone on the thyroid axis are related to its iodine content (previously described) and to amiodarone itself (Table 3).
Successive deiodination is the main metabolic pathway of thyroid hormones, yielding active and inactive metabolites17. Initial T4 deiodination can occur at the outer ring producing T3 (3, 3´, 5 T3), or at the inner ring forming reverse T3 (3, 3´, 5´ T3). Less than 20% of total T3 is produced in the thyroid; the rest results from deiodination in peripheral tissues17.
Deiodination of thyroid hormones is catalyzed by deiodinase isoenzymes (DI, DII, DIII)17. Amiodarone inhibits DI activity in peripheral tissues, which results in a 30% decrease in serum concentrations of T3 and increases of 20-40% in T4 levels and of 20% in reverse T3. In turn, inhibition of DII activity at pituitary level is responsible for increased TSH serum levels18.
Amiodarone also decreases intracellular T4 transport and T3 binding to its nuclear receptors.
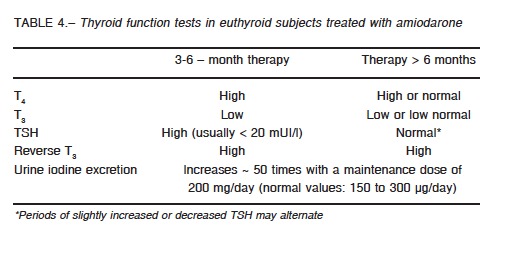
As a result of these actions, patients treated with amiodarone show alterations in thyroid hormones and TSH serum levels. These changes should be distinguished from a real dysfunction of the thyroid axis which may also occur during treatment19. Table 4 shows the laboratory alterations of the thyroid axis induced by amiodarone according to length of treatment.
Amiodarone-induced hypothyroidism (AIH)
Amiodarone-induced hypothyroidism usually appears within the first 6-18 months of treatment. It is more frequent among women, elderly patients, those with pre-existing autoimmunity and in areas with sufficient iodine intake. It can be observed in about 5-25% of treated patients20, and it is often secondary to the presence of a smaller thyroid reserve, due to underlying autoimmune thyroiditis, treatment with 131I, thyroid surgery, or the presence of predisposing chronic diseases, such as thalassemia major21. Clinical manifestations do not differ from those observed in primary hypothyroidism. Amiodarone-induced hypothyroidism, if sustained or severe, may induce ventricular arrhythmias18. Less commonly, it has been associated with acute renal insufficiency, which is reversible after treatment with levothyroxine and discontinuation of amiodarone22. It should be pointed out that amiodarone-induced hypothyroidism does not depend on the dosage of amiodarone administered. Amiodarone concentration and its cumulative doses do not differ between patients who remain euthyroid and those who develop hypothyroidism in the course of treatment with amiodarone15. Spontaneous remission of amiodarone-induced hypothyroidism does not occur if treatment with amiodarone is continued. In patients with
previously normal thyroid function, interruption of the drug promotes recovery within 2-4 months in 60% of the cases. In the remaining 40%, it may persist for 5-8 months more.
In patients with previous thyroid dysfunction, hypothyroidism will persist even after discontinuation of amiodarone, requiring chronic levothyroxine therapy15.
In any of these scenarios, it is not necessary to interrupt amiodarone administration in the presence of hypothyroidism.
The decision about whether to treat amiodarone-induced hypothyroidism or not depends on the degree of dysfunction, the patient’s age and, in particular, on the underlying cardiac condition15, 18. In the presence of mild subclinical hypothyroidism (TSH < 10 uUI/ml), control without treatment may be sufficient. Low-dose levothyroxine (LT4) therapy can be initiated, starting with 25 mcg/day if treatment is required. Serum TSH levels should be assessed after 4-6 weeks, and the LT4 dose increased slowly every 4 or more weeks according to tolerance and cardiovascular controls, maintaining higher TSH levels than in other cases of hypothyroidism13.
At the other end of the amiodarone-induced hypothyroidism spectrum is myxedema coma. This condition is extremely severe and reinforces the concept of regular examinations of thyroid function in patients treated with amiodarone23. Amiodarone may also induce destructive thyroiditis due to direct cytotoxic damage of thyroid follicular cells causing thyrotoxicosis. About 15% of the cases subsequently develop hypothyroidism13.
In summary, monitoring of thyroid function is necessary in every patient that may need amiodarone treatment and should conveniently be performed before the beginning of treatment, requiring subsequent assessments after the first month, the third month, and every six months thereafter13.
3. Lithium
Lithium carbonate (Li2CO3) is an alkali cation of widespread use in neuropsychiatry. It is estimated that around 1 in 200 people receives lithium to treat bipolar disorder24. Lithium is concentrated in the thyroid in a ratio 3-4 times higher than in plasma24. It increases intrathyroidal iodine content, inhibits iodotyrosine coupling and blocks the release of thyroid hormones24. In vitro, it decreases colloid droplet formation within thyroid cells, a reflection of lower colloid pinocytosis from the follicular lumen. The inhibition of thyroid hormone secretion promotes a higher TSH secretion, which results in an increased thyroid volume. Additionally, it might induce signaling alterations in IGF-1, in other tyrosine kinases and in Wnt/beta-catenin signaling, favoring cell proliferation and the resulting goitrogenesis25. Cross-sectional studies have revealed the presence of diffuse goiter in 40-50% of patients treated with lithium within the first 5-10 years26.
The prevalence of lithium-induced hypothyroidism varies between 6 and 52% according to several series, and it is usually subclinical26, though severe hypothyroidism and also myxedema coma has been reported27. Lithium-induced hypothyroidism is more frequent among women and in the first two years of treatment24. In many cases, there is an underlying component of autoimmune thyroiditis26, 28. Treatment of hypothyroidism does not require withdrawal of lithium and is carried out with levothyroxine in usual doses. Before starting treatment with lithium, a thyroid test should be obtained and it should be repeated every 6-12 months24.
4. Minocycline
It is an antibiotic of the tetracycline group used to treat acne vulgaris. Benitz et al. initially described minocycline-induced black thyroid in 196729. Over the following decades, about 125 cases were reported in the literature30. Even though the black pigmentation of the thyroid has been considered pathognomonic of chronic minocycline intake, other tetracyclines such as doxycycline may induce it in just 12-day long treatments31. This pigmentation may also affect other tissues such as skin, sclera, bone, teeth, gingiva and nails32. The insoluble black pigment results from minocycline oxidation by thyroid peroxidase30. Minocycline may also inhibit thyroid function and may have goitrogenic effects33, which might be due to a blocking of the peroxidase activity on the coupling reaction32.
b) Immune mechanisms
The first descriptions associating thyroid dysfunction with interferon-alpha therapy (IFN alpha) date back to 198634. Its use has noticeably increased over the last few years in the treatment of diverse neoplastic and infectious entities such as leukemia, condyloma acuminatum, Kaposi’s sarcoma and, particularly, hepatitis B and C35. IFN-alpha activates a series of intracellular signals including JAK-STAT, CRK, IRS, and MAP-kinase pathways, stimulating transcription of the specific proteins responsible for mediating their antitumor immunomodulating effects34. Thus, the expression of class I proteins from the major histocompatibility complex increases and this may lead to higher exposure of autoantigens promoting thyroid damage. The mechanisms through which IFN-alpha induces thyroid dysfunction are still not clear. The recruitment of immune cells (natural killer cells) capable of damaging the thyroid or even a direct cytotoxic effect has been suggested36. One of the most common side effects of IFN-alpha is thyroiditis, described in 20-40% of cases, of which 5-20% develop thyroid dysfunction34, 37. Such complications may arise at any stage of treatment, even 6 months after discontinuation and are more common in female patients34. Persistent hypothyroidism is frequent after discontinuation of IFN-alpha38. It should be highlighted that both the presence of thyroid autoimmunity prior to treatment as well as an underlying genetic predisposition enhance the risk of developing IFN-alpha-induced autoimmune thyroiditis36, 38.
Considering the frequency of thyroid complications in patients treated with IFN-alpha, it would be advisable to request an antithyroid antibody test before starting treatment. Patients with hepatitis C are more prone to develop autoimmune and non-autoimmune thyroiditis induced by IFN-alpha since there might be a molecular mimicry phenomenon between the virus and thyroid antigens39.
Since the symptoms of hypothyroidism, such as fatigue and weight gain, may be attributed to hepatitis C or to IFN-alpha treatment, its diagnosis is usually delayed34. Treatment of INF-alpha-induced hypothyroidism should be regularly monitored (every 2-3 months) as dysfunction may be progressive requiring adjustments of the replacement dose. If treatment with INF-alpha is interrupted, it is necessary to evaluate the possibility of decreasing or even discontinuing hormone therapy34.
Other cytokines that may induce or exacerbate autoimmune thyroiditis are interferon beta40 and interleukin-241.
c) Drug-induced thyroiditis
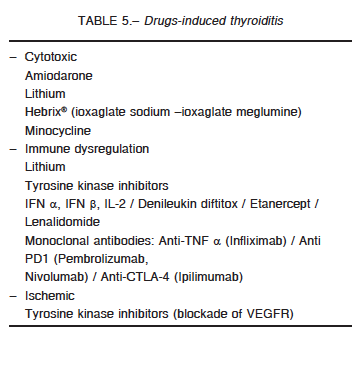
Drug-induced thyroiditis can be the result of several mechanisms, the most common being an inflammatory/destructive process induced by drugs. These alterations start with an initial thyrotoxicosis phase due to the massive release of thyroid hormones into the circulation. After this, hypothyroidism is observed, which can be transient if full restoration of the thyroid tissue occurs42, or permanent. In other cases, thyroiditis is caused by the induction of immune mechanisms or by the blocking of the vascular endothelial growth factor receptor (VEGFR), as occurs with tyrosine kinase inhibitors42. The mechanisms of drug-induced thyroiditis may be summarized as follows:
– Cytotoxic
– Immune dysregulation
– Ischemic, by blocking the vascular endothelial growth factor receptor
Table 5 provides a list of the drugs that may induce thyroiditis.
d) Mixed: tyrosine kinase inhibitors
Tyrosine kinase inhibitors may induce hypothyroidism by different or mixed mechanisms over thyroid economy42.
The first description of tyrosine kinase inhibitor-induced hypothyroidism dates back to 2005, in patients with medullary thyroid cancer treated with imatinib43. Other tyrosine kinase inhibitors responsible for inducing hypothyroidism, as seen in several published cases, are sunitinib, sorafenib, cabozantinib, vandetanib, lenvatinib, etc. Although the use of these drugs initially focused on the treatment of gastrointestinal stromal tumors and renal
carcinoma, some of them are currently approved for the treatment of metastatic differentiated thyroid cancer (lenvatinib, sorafenib) and medullary thyroid cancer (vandetanib and cabozantinib). Currently, the incidence of tyrosine kinase inhibitor-induced hypothyroidism is estimated to be present in more than 50% of cases44.
Tyrosine kinase inhibitors promote hypothyroidism through several mechanisms, the most relevant of which are:
– Ischemic thyroiditis due to a marked capillary regression caused by blocking the vascular endothelial growth factor45.
– Higher thyroid hormone metabolism due to hepatic microsomal and DIII induction4.
Further effects of tyrosine kinase inhibitors on the thyroid include: inhibition of iodine organification, inhibition of peroxidase46, blocking of iodine uptake, thyroid autoimmunity47 and alteration of the intestinal absorption and of the enterohepatic reabsorption of levothyroxine42. Around 30-35% of patients treated with tyrosine kinase inhibitors present transient increase of TSH levels which requires no treatment48. Consequently, it is advisable to perform an initial thyroid examination, followed by assessments every 4 weeks during 4 months, and finally every 2-3 months during treatment with tyrosine kinase inhibitors 49.
Mechanisms of secondary/central
drug-induced hypothyroidism
a) Inhibition of TSH synthesis
1. Bexarotene
Bexarotene is a synthetic compound that represents a new subgroup of retinoids that activate retinoid X receptors (RXRs), which can therefore be defined as a rexinoid agent. It is used in the treatment of cutaneous T-cell lymphoma and induces central hypothyroidism due to TSH suppression in 90% of cases50. Bexarotene, like T3 and 9-cis-retinoic acid, produces about 50% in vitro suppression of the gene promoter of TSH beta-subunit. It also stimulates the peripheral metabolism of thyroid hormones by induction of glucuronyl transferases and sulfotransferases51. Thus, patients with bexarotene-induced hypothyroidism usually require higher hormone replacement doses (up to two times higher)52. Hypothyroidism appears a few days after treatment is started and all patients recover thyroid axis function after discontinuation. This effect is not observed with 13-cis-retinoic acid (isotretinoin), which is used for severe acne.
2. Somatostatin analogues
With respect to thyroid axis, somatostatin analogues have demonstrated therapeutic effectiveness in patients with the syndrome of pituitary resistance to thyroid hormones and with thyrotropinomas53. Administration of somatostatin to healthy volunteers decreases both TSH pulse frequency and amplitude54. Colao et al. stated that prolonged use of somatostatin analogues reduces TSH and its response to stimulus with thyrotropin-releasing hormone without affecting serum levels of thyroid hormone55. In a review of somatostatin analogues in acromegaly, an incidence of 2% of central hypothyroidism is described56. However, it is estimated that, although somatostatin analogues suppress TSH through direct action on thyrotropes, these effects are mainly temporary and generally do not promote the appearance of central hypothyroidism57.
3. Glucocorticoids and dopamine
The influence of glucocorticoids on TSH secretion has been long acknowledged58. At physiological levels, hydrocortisone plays an important role in the diurnal variation of TSH, showing lower levels in the morning and higher levels at night54. This explains why TSH levels are high in patients with untreated adrenal insufficiency. Glucocorticoids in high doses suppress TSH in both normal and in hypothyroid subjects. A prolonged administration of glucocorticoids in high doses does not usually cause central hypothyroidism. Recent publications suggest the presence of central hypothyroidism in patients with corticotroph microadenomas produced by the suppression of the hypothalamic-pituitary-thyroid axis induced by an excess of cortisol58.
Dopamine and its agonists, such as bromocriptine, suppress TSH secretion by activating its D2 receptors57. Although the administration of dopamine or its derivatives dobutamine and dopexamine may cause difficulty in the interpretation of TSH serum levels, it does not induce central hypothyroidism. If ultrasensitive methods detecting TSH levels within the range of 0.01 mUI/ml are used, TSH values during treatment with these drugs are usually between 0.08 and 0.4 mUI/ml. These values are clearly different from those commonly observed in hyperthyroidism (TSH lower than 0.01 mUI/ml)59.
b) Immune mechanisms
1. Anti-Cytotoxic T lymphocyte associated antigen 4 (anti-CTLA-4) antibodies
Monoclonal anti-CTLA-4 antibodies are used in the treatment of several neoplasias, such as metastatic renal carcinoma and melanoma among others. The administration of ipilimumab or tremelimumab may induce the development of acute lymphocytic hypophysitis with panhypopituitarism; central hypothyroidism being the most frequent deficiency (90% of cases)60. Hypophysitis is observed in 7-13% of the patients treated with ipilimumab, who present with headache as the most frequent symptom61. It is more common in male patients with an average age of 60 and usually appears after 2 -4 months of treatment, typically after the third cycle60. The differential diagnosis is with metastatic melanoma and other pituitary tumors. A nuclear magnetic resonance can help diagnose hypophysitis by revealing pituitary enlargement with an increased longitudinal diameter, thickening of the stalk, suprasellar convexity and a hyperintense heterogeneous signal62. Ipilimumab-induced hypophysitis is generally characterized by the absence of diabetes insipidus unlike postpartum or gestational autoimmune hypophysitis62. Ipilimumab can also affect the thyroid function (though less commonly) and has been associated with primary adrenal insufficiency as well63.
2. Anti-Programmed cell death-1 receptor (anti-PD-1) antibodies
Hypophysitis induced by anti-PD-1 such as pembrolizumab and nivolumab is far more unusual, with few cases described64. On the other hand, the incidence of thyroid disorders induced by anti-PD-1 particularly silent thyroiditis is more common and occurs in 5-10% of patients64.
Interactions in the treatment of
hypothyroidism
Some drugs may reduce the intestinal absorption of levothyroxine by altering its transport and/or metabolism.
Drugs that decrease levothyroxine absorption
The gastrointestinal tract is of great importance in thyroid physiology, since conjugated iodothyronines are excreted in bile and are partially unconjugated in the intestine by bacterial enzymes, liberating a small amount of free hormones which are absorbed into portal circulation65. Less than 10% of the daily production of thyroid hormones is excreted in feces. Approximately 62-82% of orally administered levothyroxine is absorbed within the first three hours after intake, mainly in the jejunum and the ileum66. This absorption is higher when the drug is administered on an empty stomach, which shows the importance of gastric acidity in this process67. In hypothyroid patients receiving levothyroxine treatment, a wide range of drugs and dietary substances alter its absorption, preventing an adequate metabolic control68.
Colestyramine, colestipol and colesevelam are bile acid binding resins used in hyperlipidemia which significantly inhibit absorption of thyroid hormones69. Because of its potent action, colestyramine is used in the treatment of exogenous hyperthyroidism and it is sometimes recommended, combined with methimazole, for a faster control of hyperthyroidism in Graves’ disease70. Other drugs that can alter intestinal absorption of levothyroxine are sucralfate71, aluminum hydroxide72, proton-pump inhibitors73, iron salts74, calcium carbonate75, and laxatives and antacids containing magnesium76.
A reduced absorption of levothyroxine has been described when administered concomitantly with sodium sulfate polyestyrene (an ion-exchange resin used in hyperkalemia), sevelamer and lanthanum carbonate (phosphate binders), chromium77, raloxifene78, orlistat66 and tyrosine kinase inhibitors42.
The interaction of some dietary substances with thyroid hormone has become increasingly relevant due to the high consumption of bran and fiber for breakfast. Bran significantly inhibits intestinal absorption of levothyroxine79, which makes it convenient to separate bran intake from hormone intake by a few hours. Soy-containing nutritional preparations also affect intestinal absorption of thyroid hormones80. A reduced absorption of levothyroxine has been described when consumed concomitantly with herbal remedies81, prunes81 and espresso coffee82.
In all the above cases, interactions can be avoided if the administration of the hormone is separated from the intake of the above-mentioned drugs and foods by 4-6 hours66. Finally, it is worth pointing out that vitamin C may increase absorption of levothyroxine, therefore, in special cases such as gastritis, the concomitant intake of both may be convenient83.
Drugs that alter levothyroxine transport and metabolism
More than 99% of thyroid hormones circulate bound to transport proteins: thyroxine-binding globulin, transthyretin (originally called ‘thyroxine-binding prealbumin’) and albumin84. Thyroxine-binding globulin transports about 70–75% of circulating T4 and the rest is bound to transthyretin and/or albumin, while the circulating free form is lower than 0.001%85. Thus, thyroxine-binding globulin constitutes the main transport protein and the one most frequently affected by drugs86, being able to modify total serum concentrations of thyroid hormones without compromising the patient’s euthyroid state, since the free fractions are not modified85.
Estrogens increase hepatic synthesis of thyroxine-binding globulin as well as its glycosylation, delaying its clearance and increasing its serum concentration86. This increase is dose-dependent and total T4 levels rise by 20-35%84. On occasion, it could be necessary to increase the thyroid replacement dose in hypothyroid postmenopausal women undergoing estrogen therapy87. The same can be observed about the administration of oral contraceptives. These changes are usually seen within the first six weeks after starting estrogen therapy and the maximum effect is reached by week 1287. Evaluating the thyroid function 6-8 weeks after the start of oral estrogen therapy is recommended in order to adjust the levothyroxine dose. These changes are not observed in the case of transdermal estrogen therapy, due to the absence of the first hepatic stage. In short, in hypothyroid women who might require estrogen replacement therapy, transdermal delivery would be more advisable.
The interruption of estrogen therapy or the drop in estrogen levels during menopause produces the opposite effect in hypothyroid women receiving levothyroxine, thus requiring a decrease in the dose of thyroid hormone85. In hypothyroid patients who become pregnant, estrogens induce a higher levothyroxine requirement of about 40-50% above the pre-pregnancy replacement dose88. Due to their estrogenic agonist effect at hepatic level, tamoxifen and other selective estrogen receptor modulators modify the thyroid profile of hypothyroid women who may therefore, also require an adjustment of the levothyroxine dosage89.
A wide variety of drugs affect thyroid hormones metabolism, especially through intrahepatic deiodination, increased activity of CYP3A4, and conjugation with sulfate and glucoronic acid (enzyme induction). The main drugs involved are phenobarbital, carbamazepine, rifampicin and phenytoin90-92. In healthy subjects, the hypothalamic-pituitary-thyroid axis compensates for this situation increasing the production and secretion of thyroid hormones, and T4, T3 and TSH remain normal. In hypothyroid patients, this compensatory mechanism fails and it may be necessary to increase levothyroxine replacement doses.
In conclusion, the aim of this review is to draw attention to some major aspects of clinical practice that may go unnoticed. For example, when drugs such as amiodarone, lithium or immunomodulators are to be prescribed, the thyroid function should be previously assessed and regularly monitored thereafter.
It is also necessary to bear in mind that the intake of levothyroxine should be separated from that of drugs or foods that may impair its absorption. Similarly, those drugs that interfere with the transport and metabolism of the exogenous hormone should be taken into account and the corresponding dose adjustments should be made in hypothyroid patients.
Further consideration should be given to those drugs that alter thyroid function tests leading to false diagnoses and unnecessary therapies.
Finally, the new biological immunomodulating and antineoplastic therapies enlarge the battery of drugs which substantially interact with thyroid function and endocrine activity in general.
Acknowledgements: The authors wish to express their gratitude to Professor Leonard Wartofsky, MD, MACP, Georgetown University School of Medicine, Department of Medicine, Washington Hospital Center, for the revision of this article.
Conflict of interests: Leonardo F. L. Rizzo, is Medical Director of Química Montpellier S.A. Daniela Mana and Hector Serra, are Medical Consultants for Química Montpellier S.A.
References
1. Rizzo L, Serra HA, Niepomniszcze H. Alteraciones de la función tiroidea inducidas por fármacos. Rev Arg Med 2000; 2: 67-78.
2. Rizzo L. Hipotiroidismo inducido por fármacos. En: Niepomniszcze H, Novelli JL (eds) Hipotiroidismo. UNR Editora: Rosario, 2009, p 215-23.
3. Sawin CT. Edwin B. Astwood. The Endocrinologist 1993; 3: 239-41.
4. Cooper DS. Antithyroid drugs. N Engl J Med 2005; 352: 905-17.
5. Medvei VC. The discovery of iodine. En: Medvei VC (ed) The History of Clinical Endocrinology. New York: Parthenon Publishing Group Inc, 1993, p 104.
6. Burman KD, Wartofsky L. Iodine effects on the thyroid gland: Biochemical and clinical aspects. Rev Endocr Metab Disord 2000; 1: 19-25.
7. Laurberg P, Pedersen KM, Hreidarsson A, Sigfusson N, Iversen E, Knudsen PR. Iodine intake and the pattern of thyroid disorders: A comparative epidemiological study of thyroid abnormalities in Iceland and in Jutland, Denmark. J Clin Endocrinol Metab 1998; 83: 765-9.
8. Philippou G, Koutras DA, Piperingos G, Souvatzoglou A, Moulopoulos SD. The effect of iodide on serum thyroid hormone levels in normal persons, in hyperthyroid patients, and in hypothyroid patients on thyroxine replacement. Clin Endocrinol (Oxf) 1992; 36: 573-8.
9. Lee SY, Rhee CM, Leung AM, Braverman LE, Brent GA, Pearce EN. A review: Radiographic iodinated contrast-induced thyroid dysfunction. J Clin Endocrinol Metab 2015; 100: 376-83.
10. Smerdely P, Lim A, Boyages SC, et al. Topical iodine-containing antiseptics and neonatal hypothyroidism in very low-birth weight infants. Lancet 1989; 2: 661-4.
11. Clark CD, Bassett B, Burge MR. Effects of kelp supplementation on thyroid function in euthyroid subjects. Endocr Pract 2003; 9: 363-9.
12. Kornelius E, Chiou JY, Yang YS, Peng CH, Lai YR, Huang CN. Iodinated contrast media increased the risk of thyroid dysfunction: A 6-year retrospective cohort study. J Clin Endocrinol Metab 2015; 100: 3372-9.
13. Rizzo LF, Bruno OD. Amiodarona y disfunción tiroidea. Medicina (B Aires) 2012; 72: 63-74.
14. Nattel S, Talajic M, Fermini B, Roy D. Amiodarone: Pharmacology, clinical actions, and relationships between them. J Cardiovasc Electrophysiol 1992; 3: 266-80.
15. Basaria S, Cooper DS. Amiodarone and the thyroid. Am J Med 2005; 118: 706-14.
16. Fukuchi H, Nakashima M, Araki R, et al. Effect of obesity on serum amiodarone concentration in Japanese patients: population pharmacokinetic investigation by multiple trough screen analysis. J Clin Pharm Ther 2009; 34: 329-36.
17. St Germain DL, Galton VA, Hernández A. Defining the roles of the iodothyronine deiodinases: Current concepts and challenges. Endocrinology 2009; 150: 1097-1107.
18. Conen-Lehman J, Dahl P, Danzi S, Klein I. Effects of amiodarone therapy on thyroid function. Nat Rev Endocrinol 2010; 6: 34-41.
19. Newman CM, Price A, Davies DW, Gray TA, Weetman AP. Amiodarone and the thyroid: a practical guide to the management of thyroid dysfunction induced by amiodarone therapy. Heart 1998; 79: 121-7.
20. Batcher EL, Tang XC, Singh BN, Singh SN, Reda DJ, Hershman JM. Thyroid function abnormalities during amiodarone therapy for persistent atrial fibrillation. Am J Med 2007; 120: 880-5.
21. Mariotti S, Loviselli A, Murenu S, et al. High prevalence of thyroid dysfunction in adult patients with beta-thalassemia major submitted to amiodarone treatment. J Endocrinol Invest 1999; 22: 55-63.
22. Luciani R, Falcone C, Principe F, Punzo G, Mené P. Acute renal failure due to amiodarone-induced hypothyroidism. Clin Nephrol 2009; 72: 79-80.
23. Chakraborty S, Fedderson J, Gums JJ, Toole A. Amiodarone-induced mixedema coma – a case and review of the literatura. Arch Med Sci 2014; 6: 1263-7.
24. Lazarus JH. Lithium and thyroid. Best Pract Res Clin Endocrinol Metab 2009; 23: 723-33.
25. Rao AS, Kremenevskaja N, Resch J, Brabant G. Lithium stimulates proliferation in cultured thyrocytes by activating Wnt/beta-catenin signalling. Eur J Endocrinol 2005; 153: 929-38.
26. Perrild H, Hegedus L, Baastrup PC, Kayser L, Kastberg S. Thyroid function and ultrasonically determined thyroid size in patients receiving long-term lithium treatment. Am J Psychiatry 1990; 147: 1518-21.
27. Mir SA, Wani AI, Masoodi SR, Bashir MI, Ahmad N. Lithium toxicity and myxedema crisis in an elderly patient. Indian J Endocrinol Metab 2013; 17: S654-6.
28. Wilson R, McKillop JH, Crocket GT, Pearson C, Jenkins C, Burns AK, Thomson JA. The effect of lithium therapy on parameters thought to be involved in the development of autoimmune thyroid disease. Clin Endocrinol (Oxf) 1991; 34: 357-61.
29. Attwood HD, Dennet X. A black thyroid and minocycline treatment. Br Med J 1976; 2: 1109-10.
30. Bann DV, Goyal N, Crist H, Goldenberg D. Black Thyroid. Ear Nose Throat J 2014; 93: E54-5.
31. Miller BT, Lewis C, Bentz BG. Black thyroid resulting from short-term doxycycline use: case report, review of the literature, and discussion of implications. Head Neck 2006; 28: 373-7.
32. Yusim A, Ghofrani M, Ocal IT, Roman S. Black thyroid syndrome. Thyroid 2006; 6: 811-2.
33. Taurog A, Dorris ML, Doerge DR. Minocycline and the Thyroid: Antithyroid effects of the drug, and the role of thyroid peroxidase in minocycline-induced black pigmentation of the gland. Thyroid 1996; 6: 211-9.
34. Tomer Y, Menconi F. Interferon induced thyroiditis. Best Pract Res Clin Endocrinol Metab 2009; 23: 703-12.
35. Ward DL, Bing-You RG. Autoimmune thyroid dysfunction induced by interferon-alfa treatment for chronic hepatitis C: Screening and monitoring recommendations. Endocr Pract 2001; 7: 193-4.
36. Hasham A, Zhang W, Lotay V, et al. Genetic analysis of interferon induced thyroiditis (IIT): evidence for a key role for MHC and apoptosis related genes and pathways. J Autoimmun 2013; 44: 61-70.
37. Mandac JC, Chaudhry S, Sherman KE, Tomer Y. The clinical and physiological spectrum of interferon-alpha induced thyroiditis: Toward a new classification. Hepatology 2006; 43: 661-72.
38. Roti E, Minelli R, Giuberti T, et al. Multiple changes in thyroid function in patients with chronic active HCV hepatitis treated with recombinant interferon-alpha. Am J Med 1996; 101: 482-7.
39. Tran A, Quaranta JF, Benzaken S, et al. High prevalence of thyroid autoantibodies in a prospective series of patients with chronic hepatitis C before interferon therapy. Hepatology 1993; 18: 253-7.
40. Caraccio N, Dardano A, Manfredonia F, et al. Long-term follow-up of 106 multiple sclerosis patients undergoing interferon-beta 1a or 1b therapy: predictive factors or thyroid disease development and duration. J Clin Endocrinol Metab 2005; 90: 4133-7.
41. Vialettes B, Guillerand MA, Viens P, et al. Incidence rate and risk factors of thyroid dysfunction during recombinant interleukin-2 therapy in advanced malignancies. Acta Endocrinol Copenh 1993; 129: 31-8.
42. Sherman SI. Tyrosine kinase inhibitors and the thyroid. Best Pract Res Clin Endocrinol Metab 2009; 23: 713-22.
43. de Groot JW, Zonnenberg BA, Plukker JT, van Der Graaf WT, Links PT. Imatinib induces hypothyroidism in patients receiving levothyroxine. Clin Pharmacol Ther 2005; 78: 433-8.
44. Torino F, Corsello SM, Longo R, Barnabei A, Gasparini G. Hypothyroidism related to tyrosine kinase inhibitors: an emerging toxic effect of targeted therapy. Nat Rev Clin Oncol 2009; 6: 219-28.
45. Makita N, Iri T. Tyrosine kinase inhibitor-induced thyroid disorders: A review and hypothesis. Thyroid 2013; 23: 151-9.
46. Wong E, Rosen LS, Mulay M, et al. Sunitinib induces hypothyroidism in advanced cancer patients and may inhibit thyroid peroxidase activity. Thyroid 2007; 17: 351-5.
47. Pani F, Atzori F, Baghino G, et al. Thyroid dysfunction in patients with metastatic carcinoma treated with sunitinib: is thyroid autoimmunity involved? Thyroid 2015; 25: 1255-61.
48. Wolter P, Stefan C, Decallonne B, et al. The clinical implications of sunitinib-induced hypothyroidism: a prospective evaluation. Br J Cancer 2008; 99: 448-54.
49. Hamnvik OP, Larsen PR, Marqusee E. Thyroid dysfunction from antineoplastic agents. J Natl Cancer Inst. 2011; 103: 1572-87.
50. Torino F, Corsello SM, Salvatori R. Endocrinological side-effects of immune checkpoint inhibitors. Curr Opin Oncol. 2016; 28: 278-87.
51. Sherman SI, Gopal J, Haugen BR, et al. Central hypothyroidism associated with retinoid X receptor-selective ligands. N Engl J Med 1999; 340: 1075-9.
52. Smit JWA, Stokkel MPM, Pereira AM, Romijn JA, Visser TJ. Bexarotene-induced hypothyroidism: Bexarotene stimulares the peripheral metabolism of thyroid hormones. J Clin Endocrinol Metab 2007; 92: 2496-9.
53. Beck-Peccoz P, Persani L, Mannavola D, Campi I. Pituitary tumours: TSH-secreting adenomas. Best Pract Res Clin Endocrinol Metab 2009; 23: 597-606.
54. Samuels MH. Effects of variations in physiological cortisol levels on thyrotropin secretion in subjects with adrenal insufficiency: a clinical research center study. J Clin Endocrinol Metab 2000; 85:1388-93.
55. Colao A, Merola B, Ferone D, et al. Acute and chronic effects of octreotide on thyroid axis in growth hormone-secreting and clinically non-functioning pituitary adenomas. Eur J Endocrinol 1995; 133: 189-94.
56. Freda PU. Somatostatin analogs in acromegaly. J Clin Endocrinol Metab 2002; 77: 3013-8.
57. Haugen BR. Drugs that supress TSH or cause central hypothyroidism. Best Pract Res Clin Endocrinol Metab 2009; 23: 793-800.
58. Mathiodakis N, Thapa S, Wand GS, Salvatori T. ACTH-secreting pituitary microadenomas are associated with a higher prevalence of central hypothyroidism compared to other microadenoma types. Clin Endocrinol (Oxf) 2012; 77: 871-6.
59. Baloch Z, Carayon P, Conte-Devolx B, et al. Guidelines Committee, National Academy of Clinical Biochemistry Laboratory medicine practice guidelines. Laboratory support for the diagnosis and monitoring of thyroid disease. Thyroid 2003; 13: 3-126.
60. Dadu R, Zobniw C, Diab A. Managing adverse events with immune checkpoint agents. Cancer J 2016; 22: 121-9.
61. Faje A. Immunotherapy and hypophysitis: clinical presentation, treatment, and biologic insights. Pituitary 2016; 19: 82-92.
62. Albarel F, Gaudy C, Castinetti F, et al. Long-term follow-up of ipilimumab-induced hypophysitis, a common adverse event of the anti-CTLA-4 antibody in melanoma. Eur J Endocrino 2015; 172: 195-204.
63. Corsello SM, Barnabei A, Marchetti P, De Vecchis L, Salvatori R, Torino F. Endocrine side effects induced by immune checkpoint inhibitors. J Clin Endocrinol Metab 2013; 98: 1361-75.
64. González-Rodríguez E, Rodríguez-Abreu D. Immune checkpoint inhibitors: review and management of endocrine adverse effects. Oncologist 2016; 21: 804-16.
65. Hays MT. Thyroid hormone and the gut. Endocr Res 1988; 14: 203-24.
66. Benvenga S, Bartolone L, Squadrito S, Lo Giudice F, Trimarchi F. Delayed intestinal absorption of levothyroxine. Thyroid 1995; 5: 249-53.
67. Bach-Huynh TG, Nayak B, Loh J, Soldin S, Jonklaas J. Timing of levothyroxine administration affects serum thyrotropin concentration. J Clin Endocrinol Metab 2009; 94: 3905-12.
68. McMillan M, Rotenberg KS, Vora K, et al. Comorbidities, concomitantat medications, and diet as factors affecting levothyroxine therapy: Results of the CONTROL surveillance project. Drugs R D 2016; 15: 53-68.
69. Harmon SM, Seifert CF. Levothyroxine – cholestyramine interaction reemphasized. Ann Intern Med 1991; 115: 658-9.
70. Mercado M, Mendoza-Zubieta V, Bautista-Osorio R, Espinoza-De Los Monteros AL Treatment of hyperthyroidism with a combination of methimazole and cholestytamine. J Clin Endocrinol Metab 1996; 81: 3191-3.
71. Campbell JA, Schmidt BA, Bantle JP. Sucralfate and the absorption of L-thyroxine. Ann Intern Med 1994; 121: 152.
72. Liel Y, Sperber AD, Shany S. Nonespecific intestinal absorption of levothyroxine by aluminum hydroxide. Am J Med 1994; 97: 363-5.
73. Sachmechi I, Reich DM, Aninyei M, Wibowo F, Gupta G, Kim PJ. Effect of proton pump inhibitors on serum thyroid-stimulating hormone level in euthyroid patients treated with levothyroxine for hypothyroidism. Endocr Pract 2007; 13: 345-9.
74. Campbell NR, Hasinoff BB, Stalts H, Rao B, Wong NC. Ferrous sulfate reduces thyroxine efficacy in patients with hypothyroidism. Ann Intern Med 1992; 117: 1010-3.
75. Singh N, Weisler SL, Hershman JM. The accute effect of calcium carbonate on the intestinal absorption of levothyroxine. Thyroid 2001; 11: 967-71.
76. Mersebach H, Rasmussen AK, Kirkegaard L, Feldt-Rasmussen U. Intestinal adsorption of levothyroxine by antacids and laxatives: case stories and in vitro experiments. Pharmacol Toxicol 1999; 84:107-9.
77. John-Kalarickal J, Pearlman G, Carlson HE. New medications which decrease levothyroxine absorption. Thyroid 2007; 17: 763-5.
78. Garwood CL, Van Schepen KA, McDonough RP, Sullivan AL. Increased thyroid-stimulating hormone levels associated with concomitant administration of levothyroxine and raloxifene. Phamacotherapy 2006; 26: 881-5.
79. Liel Y, Harman-Boehm I, Shany S. Evidence for a clinically important adverse effect of fiber-enriched diet on the bioavailability of levothyroxine in adult hypothyroid patients. J Clin Endocrinol Metab 1996; 81: 857-9.
80. Bell DS, Ovalle F. Use of soy protein supplement and resultant need for increased dose of levothyroxine. Endocr Pract 2001; 7: 193-4.
81. Geatti O, Barkan A, Turrin D, Orsolon PG, Shapiro B. L-Thyroxine malabsorption due to the ingestion of herbal remedies. Thyroidol Clin Exp 1993; 5: 97-102.
82. Benvenga S, Bartolone L, Pappalardo MA, et al. Altered intestinal absorption of L-thyroxine caused by coffee. Thyroid 2008; 18: 293-301.
83. Antúnez PB, Licht SD. Vitamin C improves the apparent absorption of levothyroxine in a subset of patients receiving this hormone for primary hypothyroidism. Rev Argent Endocrinol Metab 2011; 48: 16-24.
84. Dufour DR. Laboratory tests of thyroid function: Uses and limitations. Endocrinol Metab Clin N Am 2007; 36: 579-94.
85. Tahboub R, Arafah BM. Sex steroids and the thyroid. Best Pract Res Clin Endocrinol Metab 2009; 23: 769-80.
86. Bartalena L, Robbins J. Variations in thyroid hormone transport proteins and their clinical implications. Thyroid 1992; 2: 237-45.
87. Arafah BM. Increased need for thyroxine in women with hypothyroidism during estrogen therapy. N Engl J Med 2001; 344: 1743-9.
88. Alexander EK, Marqusee E, Lawrence J, Jarolim P, Fischer GA, Larsen PR. Timing and magnitude of increases in levothyroxine requirements during pregnancy in women with hypothyroidism. N Engl J Med 2004; 351: 241-9.
89. Anker GB, Lonning PE, Aakvaag A, Lien EA. Thyroid function in postmenopausal breast cancer patients treated with tamoxifen. Scan J Clin Lab Invest 1998; 58: 103-7.
90. Cavalieri RR, Sung LC, Becker CE. Effects of phenobarbital on thyroxine and triyodothyronine kinetics in Graves’ disease. J Clin Endocrinol Metab 1973; 37: 308-16.
91. Surks MI, DeFesi CR. Normal serum free thyroid hormone concentrations in patients treated with phenytoin or carbamazepine. JAMA 1996; 275: 1495-8.
92. Isley WL. Effect of rifampin therapy on thyroid function tests in a hypothyroid patient on replacement L-thyroxine. Ann Intern Med 1987; 107: 517-8.
– – – –
NIVEL, A
“Usted enfoca el problema ingreso a nivel del estudiantado”. “Enfoquemos el análisis a nivel grupal”.
Adolfo Bioy Casares (1914-1999)
Breve diccionario del argentino exquisito. Buenos Aires: Emecé, 1978, p 103
