M. VICTORIA SALGADO 1, PAM COXSON 2, 3, JONATAN KONFINO 1, JOANNE PENKO 2, 3, VILMA E. IRAZOLA 4, 5, LAURA GUTIÉRREZ 4, 5, ALICIA FERNÁNDEZ 6, RAÚL MEJÍA 1
1 Centro de Estudios de Estado y Sociedad (CEDES), Buenos Aires, Argentina, 2 Center for Vulnerable Populations, University of California San Francisco, San Francisco, California, USA, 3 Department of Epidemiology and Biostatistics, University of California San Francisco, San Francisco, California, USA, 4 Instituto de Efectividad Clínica y Sanitaria (IECS), Buenos Aires, Argentina, 5 Centro de Excelencia en Salud Cardiovascular para América del Sur (CESCAS), Buenos Aires, Argentina, 6 Department of Medicine, University of California San Francisco, San Francisco, California, USA
Resumen La enfermedad cardiovascular (ECV) es la principal causa de muerte en Argentina. Los modelos de simulación por computadora permiten extrapolar evidencia a poblaciones más amplias que las originalmente estudiadas, a lo largo de períodos prolongados, y comparar diferentes subpoblaciones. El Cardiovascular Disease Policy Model (CVDPM, por sus siglas en inglés) es un modelo de simulación utilizado para representar y proyectar la mortalidad y morbilidad por ECV en la población de 35 o más años. El objetivo de este trabajo fue actualizar la versión argentina del CVDPM. Para esto, se utilizó información del Censo Nacional 2010, la Encuesta Nacional de Factores de Riesgo 2013, el estudio CESCAS I, y el estudio PrEViSTA, para ctualizar la dinámica del tamaño de la población, sus características demográficas, y la distribución de factores de riesgo cardiovasculares a lo largo del tiempo. Las proyecciones del modelo se calibraron comparándolas con información sobre eventos de ECV y mortalidad en el año 2010 (año de referencia) en Argentina. Las estadísticas argentinas informaron que en 2010 la población de 35 o más años sufrió un total de 41 219 infartos de miocardio (IM), 58 658 accidentes cerebrovasculares y 281 710 muertes totales. El CVDPM predijo 41 265 IM (diferencia: 0.11%), 58 584 accidentes cerebrovasculares (diferencia: 0.13%) y 280 707 muertes totales (diferencia: 0.36%). En todos los casos, la versión final del modelo predijo el número real de eventos cardiovasculares con una precisión superior al 99.5%, pudiendo ser utilizado para pronosticar cambios en la incidencia y mortalidad de ECV debidos de la implementación de políticas públicas.
Palabras clave: modelos de simulación por computadora, enfermedad cardiovascular, Argentina, salud pública, políticas de salud
Abstract Cardiovascular disease (CVD) is the leading cause of death in Argentina. Computer simulation models allow to extrapolate evidence to broader populations than the originally studied, over longer timeframes, and to compare different subpopulations. The Cardiovascular Disease Policy Model (CVDPM) is a computer simulation state transition model used to represent and project future CVD mortality and morbidity in the population 35 years-old and older. The objective of this study was to update Argentina’s version of the CVDPM. For this purpose, information from the 2010 National Census, the 2013 National Risk Factor Survey, CESCAS I study, and PrEViSTA study were used to update the dynamics of population size, demographics, and CVD risk factor distributions over time. Model projections were later calibrated by comparing them to actual data on CVD events and mortality in the year 2010 (baseline year) in Argentina. Country statistics for people 35 years-old and older reported for 2010 a total of 41 219 myocardial infarctions (MIs), 58 658 strokes, and 281 710 total deaths. The CVDPM, in turn, predicted 41 265 MIs (difference: 0.11%), 58 584 strokes (difference: 0.13%), and 280 707 total deaths (difference: 0.36%) in the same population. In all cases, the final version of the model predicted the actual number of events with an accuracy superior to 99.5%, and could be used to forecast the changes in CVD incidence and mortality after the implementation of public policies.
Key words: computer simulation models, cardiovascular diseases, Argentina, public health, health policy
Postal address: María Victoria Salgado, Centro de Estudios de Estado y Sociedad, Sánchez de Bustamante 27, 1173 Buenos Aires, Argentina
e-mail: mariavictoria.salgado@gmail.com
Non-communicable chronic diseases (NCDs) caused an estimated 39.5 million deaths in 2015, representing 70% of all deaths worldwide 1. Argentina is not an exception and cardiovascular diseases (CVD), the leading cause of death, were responsible for 28.9% of deaths in 2015 2. Clinical trials are still considered to be the gold standard for best practice evidence regarding cardiovascular disease, but due to the limited selected subset of individuals with whom these trials are conducted on, their applicability to evaluate health intervention effects on entire populations (i.e.: countries) has been questioned 3. Computer simulation models can assist with this problem, by scaling up evidence to a broader, more diverse population, and by extending intervention follow-up over longer timeframes 3. They can also be used to compare different subpopulations, or to compare effects of different interventions within the same population 3.
The Cardiovascular Disease Policy Model (CVDPM) is a computer simulation state transition model used over the past three decades to represent cardiovascular disease and to project future CVD mortality and morbidity in the United States 4-9. In recent years, the CVD Policy Model structure has been adapted to represent other nations including Argentina, Mexico and China, using nation- specific demographic, risk factor, and hospital data as well as calibration to national measures of CVD incidence, prevalence and mortality 10-12.
Argentina’s version of this model was first developed in 2009 in collaboration with researchers from Argentina’s National Ministry of Health and from University of Buenos Aires and was used to project the potential impact of public health policies aimed relating to salt consumption 13,14 tobacco smoke exposure 15 and access to HMG CoA inhibitors at the primary care level 16.
The CVD Policy Model-Argentina (CVDPM-AR) has been recently updated, incorporating newly available epidemiologic and demographic data that better reflect contemporary CVD in Argentina. Here we describe the methodology used for updating the Argentinean version of the CVD Policy Model.
Materials and methods
The CVD Policy model (Fig. 1) is a computer simulation, state transition (Markov) model that estimates the prevalence and incidence of cardiovascular disease, as well as its associated mortality and direct health care costs, by using epidemiological data of the population 35 years old and older (Fig.1) 3. The model separates the population into those without prior coronary heart disease (angina, myocardial infarction, and arrest) or stroke and those with prior CVD. The population without prior CVD is divided into cells defined by age, sex, and levels of CVD risk factors including systolic blood pressure (SBP), HDL and LDL cholesterols (HDL-c and LDL-c), smoking status, diabetes status, and body mass index (BMI). In annual cycles, the model predicts the incidence of coronary heart disease, stroke, and death due to non-cardiovascular causes as a function of age, sex, and levels of CVD risk factors. In those who develop incident disease, the model characterizes the incident event along with its sequelae for 30 days.
In the population with a history of CVD, the model predicts subsequent cardiovascular events and procedures along with deaths from cardiovascular and non-cardiovascular causes as a function of age, sex, and prior CVD history. The CVD Policy Model–Argentina includes prevalence and mean values for the following CVD risk factors cutoffs, stratified by sex and age decile (from 35-44 years old through 85-94 years old): SBP: < 130; 130-139.9; ≥ 140 mmHg; LDL: < 100; 100-129.9; ≥ 130 mg/dl; HDL: <40; 40-59.9; ≥ 60 mg/dl; smoking: active, passive, and non-smoking; diabetes: yes or no; BMI: < 25; 25-29.9; ≥ 30 kg/m2.
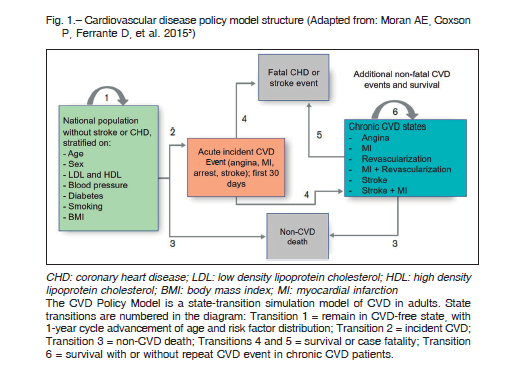
Risk factor interventions are modeled by changing the base level means of these risk factors.
Every adult alive in a given simulation year must be in a healthy or diseased state, and their risk is distinctively calculated according to their age, gender, and risk factors. Each simulation is run on an annual basis, with new 35-year-olds entering and those aging to 95 years exiting each cycle. As such, outcomes change over time according to dynamics of population size, demographics, and risk factor distributions over time 4, 9.
A more detailed description of the model is available in previous publications 3, 4.
An original version of Argentina’s CVD Policy Model was developed in 2009. Since then, new sources of information have become available:
-The National Census conducted in 2010 was used to update 2010 Argentina’s population, and to estimate the 35 yearsold people entering into the model each year up to 2100 17, 18.
-The 2013 National Risk Factor Survey was used to update age and sex-specific means and distributions for BMI, smoking and diabetes 19.
-The CESCAS I study (Study for the detection and follow up of cardiovascular disease risk factors in the southern cone of Latin America), led by the South American Center of Excellence for Cardiovascular Health, is an on-going observational prospective cohort designed to study cardiovascular disease prevalence and risk factors in Southern Latin America. This study provided information on age and sex specific means and prevalence for LDL, HDL and SBP 20,21.
-The Program for the epidemiological evaluation of stroke in Tandil (PrEViSTA) study reports local information on First-Ever Stroke and Transient Ischemic Attack Incidence 22.
After risk factors and demographic inputs are updated, the model is calibrated to reproduce contemporary cardiovascular disease morbidity and mortality data.
Argentina’s population and risk factor distribution determined the rate of incident cardiovascular events (first events in the population without disease) with the multivariate effect of the risk factor distribution based on Cox proportional hazards models of data from the ongoing Framingham Heart Study and Framingham Offspring Cohort 23, 24. We gathered local information on the number of CVD events as well as CVD mortality for the year 2010 to use as standards for calibrating model transition rates (calibration targets). CVD, non-CVD, and total deaths (by age and gender) per year were estimated from Argentina’s National Vital Statistics for the year 2010. The actual total number of deaths attributable to coronary heart disease was estimated as a compound of both definite CHD deaths (codes I20-I25 of the International Classification of Diseases, 10th Revision 25) in health records plus a percentage of poorly defined deaths (named ‘garbage’ codes, already defined) that could be attributed to CHD deaths 15, 26. Garbage codes are codes assigned to deaths that were supposedly misclassified as non-CHD deaths when they should have been coded as CHD deaths. The total number of deaths obtained was later corrected by a factor determined for countries with low quality of registry (such as Argentina) in the Global Burden of Disease initiative 27. A similar method was then used to compare predicted and reported stroke deaths (using codes I60-I69).
In the absence of national data on the absolute total number of events for myocardial infarction (MI), arrest, or stroke, by age group and gender by year, calibration targets were determined using a combination of local studies (such as the SCAR study (Síndromes Coronarios Agudos en Argentina) 28, a multicenter registry of CHD events in Argentina, and the already mentioned PrEViSTA Study) and US event rates to infer event totals for calibration targets.
Initial event rates in the population with prevalent cardiovascular disease were assumed from the prior Argentina model version and were adjusted iteratively to match the 2010 estimates of events, after subtracting the risk predicted incident events (events in the population without CVD). Then, for each of the events being analyzed, numbers obtained from calibration targets were compared to model estimations, calculating the ratio between both. These ratios were later applied to the model formulas, in order to bring its prediction closer to calibration targets. Then, a new simulation was run to check if the model fits real statistics. This iterative process was repeated until the model predictions adjusted to the
calibration targets.
The baseline year for the current version of the CVDPMAR is 2010, and all model parameters were calibrated to meet targets estimated for 2010.
Results
After the process of calibration, real and simulated total number of events and deaths due to MIs, arrest or strokes were compared, as well as total and non-CVD mortality.
Table 1 presents the difference between model predictions (estimated as described before) and national statistics following calibration. Total number of MIs, arrests and strokes were predicted with an accuracy superior to 99.8%.
In all cases, the final version of the model predicted the actual number of events with an accuracy superior to 99.5%.
The accuracy was also checked for the same outcomes but stratified by gender and age category; as an example, results for total number of MIs and mortality due to MIs can be seen in Table 2.
Accuracy was once again higher than 99.5%. Accuracy superior to 99% was also seen when comparing the predicted total number of strokes against the actual number of events, stratified by age and gender (data not shown).
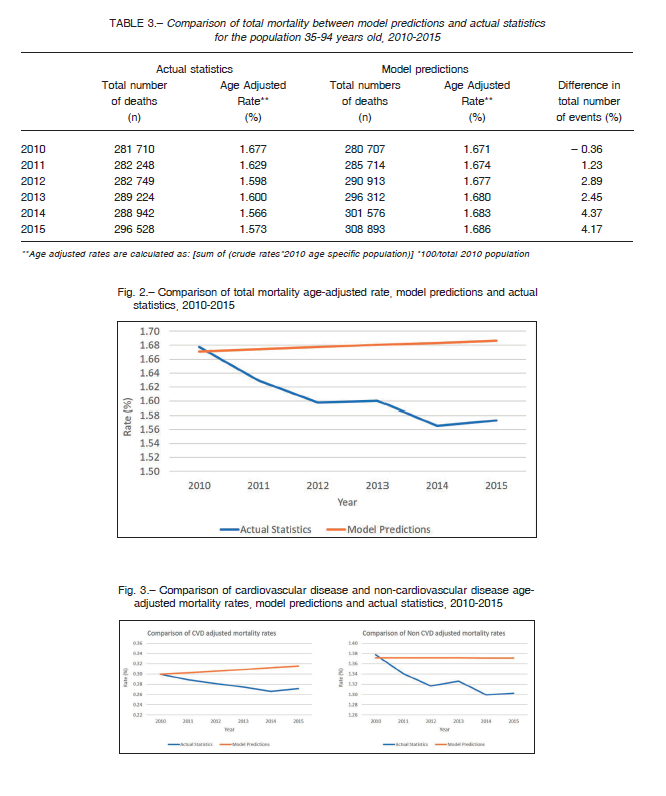
Although the model is conceived to be calibrated in the baseline year (in this case, 2010), an all-cause mortality comparison was conducted for the years 2010-2015.
Results are presented in Table 3 and Figure 2.
Figure 3 shows the same comparison but divided by CVD and Non-CVD mortality.
Figure 2 shows that, although there is a gap between actual statistics and model predictions, the absolute difference in mortality rates (total mortality, CVD and Non-CVD mortality) is not bigger than 0.12. Figure 3 shows that the slight overall increase in mortality rate in the model is due to an increase in CVD mortality. The decline in mortality seen in vital statistics is small but still many times greater than in the model and this may reflect real changes in risk.
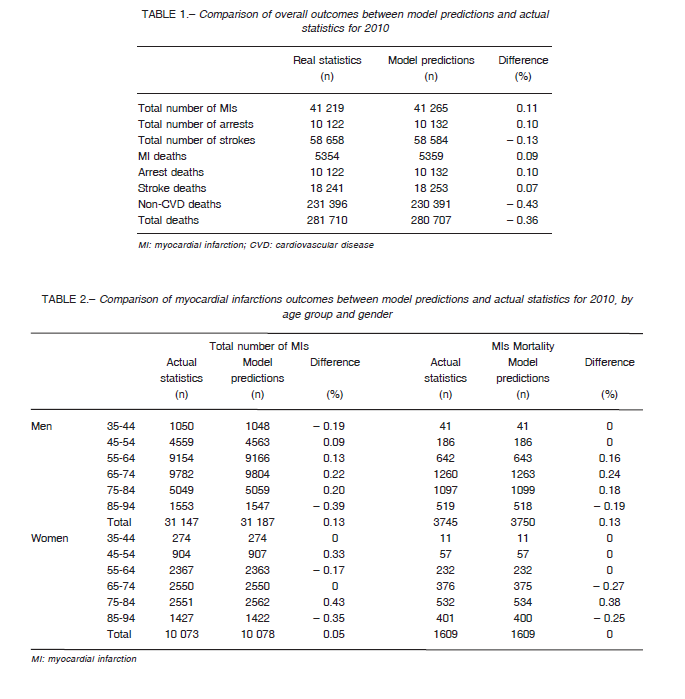
Figure 3 also shows that, while non-CVD mortality rate remains stable over the years, CVD mortality has a slight upward trend. It is important to understand that the model assumes that age-specific risk factor prevalence, and hence incidence of CVD and rates of non-CVD death, remain stable over the years in a baseline simulation. The number of incident events in the model’s baseline (no intervention) predictions is only changing as a response to changes in the population’s size and age distribution while incidence rates are steady. Prevalence of CVD is not controlled by the model and changes in response to changes in incidence; but while the model intrinsically increases CVD incidence with age, Argentina data (as reported by the National Risk Factor Survey) suggest that CVD prevalence remains almost stable among people older than 64 years old. The increase in incidence with a stable prevalence at the beginning is solved by the model by pushing up CVD prevalence in the first years after the baseline simulation, with the subsequent increase in CVD mortality. Nevertheless, the upward trend in CVD mortality is quite small (0.003% increase per year), and CVD prevalence reaches a steady state after a 10-year running (year 2020; data not shown).
Additionally, the model’s age-adjusted overall mortality rates in Table 3 remain relatively stable and that means that model assumptions are properly working.
Discussion
The updated version of the CVD Policy Model predicts accurately the occurrence of CVD events in Argentina in the year 2010, the baseline year, and could be used to forecast the changes in CVD after the implementation of public policies.
Modeling studies represent an important addition to traditional health effects and health economics studies, such as cost-effectiveness analysis, in which the impact of a specific intervention is usually evaluated through their effect in a single outcome in a limited population 29.
Modeling studies allow to expand both the population in question as well to analyze the effect of an intervention in more than one outcome, providing evidence-based support for health policy makers and government authorities 29.
Although other modelling studies have been used in Argentina 30,31, the presented version of the CVDPM not only uses the most updated information, but also incorporates input data based on national samples as well as biological measures (instead of self-reported ones) for estimating mean values of CVD risk factors. The CVD Policy Model in particular has also been described by The Pan American Health Organization to evaluate the impact of an intervention on cardiovascular disease nationwide 3.
We need to acknowledge some limitations. All modelling studies are as good as the integrity of their inputs. We used the best available data for Argentina to adapt the model, and in the case of some inputs we had to assume local or provincial data as nationally representative.
Additionally, the coefficients used to estimate the relative risk of developing cardiovascular disease for each possible risk factor combination have been taken from the Framingham study, study conducted in a mostly Anglo-Saxon population in of the United States 32. Nevertheless, there is evidence that the associations between risk factors and events are the same across different populations 33, 34.
Last, as it was mentioned, the CVDPM assumes that incidences and risk factor distributions remain stable. But CVD mortality seems to be lowering in Argentina; this could be due to multiple factors, such as a decrease in the prevalence of CVD risk factors or increased treatment effect (due to better diagnosis, more adherence, etc.). Regardless of the cause for this decrease, the model is intrinsically not able to predict changes in these factors over time. For future analysis, it is important to consider that, in this scenario, the total number of deaths may be overestimated.
Nevertheless, the CVDPM has shown to accurate predict events at the baseline year, and in case of overestimations a sensitivity analysis can be conducted, adjusting for the resulting ratios. Argentina has already used the CVDPM to inform national policies such as tobacco control, salt reduction intervention and lipid lowering programs13-16. This new version of the model can be used to continue applying an evidence-based approach on which to base health policy related decisions.
Acknowledgments: We thank Kirsten Bibbins-Domingo, PhD, MD, MAS, at University of California San Francisco, for her assistance and advice during the development of this study.
This paper is part of a research on sugar sweetened beverages consumption in Argentina, financed by the International Development Research Centre (https://www.idrc.ca), Grant N885.
Conflict of interest: None to declare
References
1. Global Health Observatory (GHO) data: Deaths from NCDs 2015. In: http://www.who.int/gho/ncd/mortality_morbidity/ncd_total/en/; accessed May 2017.
2. Ministerio de Salud de la Nación, Secretaría de Políticas Regulación e Institutos, Dirección de Estadísticas e Información de Salud. Estadísticas vitales. Información básica. Argentina ‐ Año 2015, 2016.
3. Moran AE, Coxson P, Ferrante D, et al. The Cardiovascular Disease Policy Model: Using a National Cardiovascular Disease Simulation Model to Project the Impact of National Programs to Lower Dietary Salt. In: Legetic B, Cecchini M, eds. Applying Modeling to Improve Health and Economic Policy Decisions in the Americas: The Case of Noncommunicable Diseases. Washington DC, USA: Organisation for Economic Co-operation and Development, Pan American Health Organization, World Health Organization; 2015.
4. Weinstein MC, Coxson PG, Williams LW, Pass TM, Stason WB, Goldman L. Forecasting coronary heart disease incidence, mortality, and cost: the Coronary Heart Disease Policy Model. Am J Public Health 1987; 77: 1417-26.
5. Gaspoz JM, Coxson PG, Goldman PA, et al. Cost effectiveness of aspirin, clopidogrel, or both for secondary prevention of coronary heart disease. N Engl J Med 2002; 346: 1800-6.
6. Heller DJ, Coxson PG, Penko J, et al. Evaluating the impact and cost-effectiveness of statin use guidelines for primary prevention of coronary heart disease and stroke. Circulation 2017; 136: 1087-98.
7. Lazar LD, Pletcher MJ, Coxson PG, Bibbins-Domingo K, Goldman L. Cost-effectiveness of statin therapy for primary prevention in a low-cost statin era. Circulation 2011; 124: 146-53.
8. Moise N, Huang C, Rodgers A, et al. Comparative costeffectiveness of conservative or intensive blood pressure treatment guidelines in adults aged 35-74 years: the cardiovascular disease policy model. Hypertension 2016; 68: 88-96.
9. Bibbins-Domingo K, Coxson P, Pletcher MJ, Lightwood J, Goldman L. Adolescent overweight and future adult coronary heart disease. N Engl J Med 2007; 357: 2371-9.
10. Moran A, Degennaro V, Ferrante D, et al. Coronary heart disease and stroke attributable to major risk factors is similar in Argentina and the United States: the Coronary Heart Disease Policy Model. Int J Cardiol 2011; 150: 332-7.
11. Moran A, Zhao D, Gu D, et al. The future impact of population growth and aging on coronary heart disease in China: projections from the Coronary Heart Disease Policy Model-China. BMC Public Health 2008; 8: 394.
12. Sanchez-Romero LM, Penko J, Coxson PG, et al. Projected impact of Mexico’s Sugar-Sweetened Beverage
Tax Policy on diabetes and cardiovascular disease: A Modeling Study. PLoS Med 2016; 13: e1002158.
13. Ferrante D, Konfino J, Mejia R, et al. The cost-utility ratio of reducing salt intake and its impact on the incidence of cardiovascular disease in Argentina. Rev Panam Salud Publica 2012; 32: 274-80.
14. Konfino J, Mekonnen TA, Coxson PG, Ferrante D, Bibbins-Domingo K. Projected impact of a sodium consumption reduction initiative in Argentina: an analysis from the CVD policy model–Argentina. PLoS One 2013; 8: e73824.
15. Konfino J, Ferrante D, Mejia R, et al. Impact on cardiovascular disease events of the implementation of Argentina’s national tobacco control law. Tob Control 2014; 23: e6.
16. Konfino J, Fernandez A, Penko J, et al. Comparing strategies for lipid lowering in Argentina: An analysis from the CVD Policy Model-Argentina. J Gen Intern Med 2017; 32: 524-33.
17. Censo nacional de población, hogares y viviendas 2010: censo del Bicentenario: resultados definitivos. In: http://www.indec.gov.ar/nivel4_default.asp?id_tema_1=2&id_tema_2=41&id_tema_3=135; accesed December 2016.
18. Michele Gragnolati, Rafael Rofman, Ignacio Apella, Troiano S. Los años no vienen solos. Oportunidades y desafíos económicos de la transición demográfica en Argentina: World Bank; 2014. In: http://documents.worldbank.org/curated/en/419121468002092154/pdf/880550WP0P13310o0vienen0solos0FINAL.pdf; accessed December 2016.
19. Ministerio de Salud de la Nación. Tercera Encuesta Nacional de Factores de Riesgo Para Enfermedades No Transmisibles. Presentación de los principales resultados, 2013. In: http://www.msal.gob.ar/images/stories/bes/graficos/0000000544cnt-2015_09_04_encuesta_nacional_factores_riesgo.pdf; accessed December 2016.
20. Rubinstein AL, Irazola VE, Poggio R, et al. Detection and follow-up of cardiovascular disease and risk factors in the Southern Cone of Latin America: the CESCAS I study. BMJ open 2011; 1: e000126.
21. Rubinstein AL, Irazola VE, Calandrelli M, et al. Multiple cardiometabolic risk factors in the Southern Cone of Latin America: a population-based study in Argentina, Chile, and Uruguay. Int J Cardiol 2015; 183: 82-8.
22. Bahit MC, Coppola ML, Riccio PM, et al. First-ever stroke and transient ischemic attack incidence and 30-day casefatality rates in a population-based study in Argentina. Stroke 2016; 47: 1640-2.
23. Feinleib M, Kannel WB, Garrison RJ, McNamara PM, Castelli WP. The Framingham Offspring Study. Design
and preliminary data. Prev Med 1975; 4: 518-25.
24. Dawber TH. The Framingham Study: The Epidemiology of Atherosclerotic Disease. Cambridge, MA: Harvard
University Press; 1980.
25. International Statistical Classification of Diseases and Related Health Problems 10th Revision. 2018. In: http://apps.who.int/classifications/icd10/browse/2016/en; accessed September 2018.
26. Naghavi M, Makela S, Foreman K, O’Brien J, Pourmalek F, Lozano R. Algorithms for enhancing public health utility of national causes-of-death data. Popul Health Metr 2010; 8: 9.
27. Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJL. Global Burden of Disease and Risk Factors. Chapter 3: The Burden of Disease and Mortality by Condition: Data, Methods, and Results for 2001. New York: Oxford University Press; 2006.
28. García Aurelio MJ, Cohen Arazi H, Higa C, et al. Infarto agudo de miocardio con supradesnivel persistente del segmento ST: Registro multicéntrico SCAR (Síndromes Coronarios Agudos en Argentina) de la Sociedad Argentina de Cardiología. Rev Argent Cardiol 2014; 82: 275-84.
29. Organisation for Economic Co-operation and Development, Pan American Health Organization, World Health Organization. Applying Modeling to Improve Health and Economic Policy Decisions in the Americas: The Case of Noncommunicable Diseases. Washington DC, USA 2015.
In: http://iris.paho.org/xmlui/handle/123456789/7700; accessed December 2016.
30. Rubinstein A, Colantonio L, Bardach A, et al. Estimation of the burden of cardiovascular disease attributable to modifiable risk factors and cost-effectiveness analysis of preventative interventions to reduce this burden in Argentina. BMC Public Health 2010; 10: 627.
31. Rubinstein A, Elorriaga N, Garay OU, et al. Eliminating artificial trans fatty acids in Argentina: estimated effects on the burden of coronary heart disease and costs. Bull World Health Organ 2015; 93: 614-22.
32. About the Framingham Heart Study Participants. 2018. In: https://www.framinghamheartstudy.org/participants/index.php; accessed January 2019.
33. Cortes-Bergoderi M, Thomas RJ, Albuquerque FN, et al. Validity of cardiovascular risk prediction models in Latin America and among Hispanics in the United States of America: a systematic review. Rev Panam Salud Publica 2012; 32: 131-9.
34. D’Agostino RB, Sr., Grundy S, Sullivan LM, Wilson P. Validation of the Framingham coronary heart disease prediction scores: results of a multiple ethnic groups investigation. JAMA 2001; 286: 180-7.
