JOSÉ I. TRUCCO 1, MARIANO BERRO 1, ANA LISA BASQUIERA 2, PABLO GARCÍA 3, SEBASTIÁN YANTORNO 4, SILVINA PALMER 5, ALEJANDRO REQUEJO 6, ADRIANA VITRIÚ 7, GONZALO BENTOLILA 8, MARÍA MARTA RIVAS 1, GONZALO FERINI 2, JUAN JOSÉ GARCÍA 3, JORGE MILONE 4, GERMAN STEMMELIN 5, GREGORIO JAIMOVICH 6, CECILIA FONCUBERTA 7, JULIANA MARTINEZ ROLÓN 8, GUSTAVO D. KUSMINSKY 1 ON BEHALF OF GATMO-TC (GRUPO ARGENTINO DE TRASPLANTE DE MÉDULA ÓSEA Y TERAPIA CELULAR)
1 Hospital Universitario Austral, 2 Hospital Italiano de Buenos Aires, 3 Hospital Privado de Córdoba, 4 Hospital Italiano La Plata, 5 Hospital Británico, 6 Fundación Favaloro, 7 Instituto Alexander Fleming, 8 FUNDALEU, Argentina
Resumen Se efectuó un análisis retrospectivo de 570 pacientes adultos que recibieron un trasplante alogénico de precursores hematopoyéticos, comparando los resultados según el tipo de donante. La mediana de seguimiento fue de 1.6 años. El 60% de la población se trasplantó por leucemias agudas. Los trasplantes haploidénticos se hicieron en su mayoría en leucemia mieloide aguda y en estadios tardíos en comparación a otros donantes. La mortalidad libre de enfermedad al día +100 y a 1 año fue similar para los donantes no emparentados y haploidénticos (19% y 29% vs. 17% y 28%, respectivamente). Se obtuvieron mejores resultados con donantes relacionados idénticos (7% y 15%; p < 0.001). La recaída fue mayor en los donantes haploidénticos (tres años 46% haploidénticos, 39% relacionados idénticos, 28% no emparentados; p < 0.003). El trasplante con donante haploidéntico presentó una menor supervivencia libre de progresión y menor supervivencia global a tres años (32%; p < 0.001 y 42%; p < 0.001). La incidencia de enfermedad injerto contra huésped aguda fue mayor en no emparentados (51%, 35% haploidénticos, 36% relacionados idénticos; p = 0.001), sin diferencias en grados III-IV (p = 0.73) o en EICH crónica (p = 0.2). Los trasplantes con donante haploidéntico y no emparentado mantuvieron su asociación negativa con mortalidad libre de enfermedad (HR 1.95; 95%IC 1.10-3.20 y HR 2.70; 95%IC 1.63-4.46), en análisis multivariado. El trasplante haploidéntico se asoció a mayor recaída y a menor supervivencia global. Esta experiencia mostró similar mortalidad libre de enfermedad entre trasplantes con donantes haploidénticos y no emparentados. Los trasplantes relacionados idénticos mostraron menores tasas de mortalidad libre de enfermedad.
Palabras clave: trasplante alogénico de precursores hematopoyéticos, trasplante haploidéntico, mortalidad libre de enfermedad, donantes
Abstract We retrospectively analyzed 570 adult patients who received allogeneic stem cell transplantation for malignant diseases. The outcomes were compared according to donor type. Most of the patients (60%) were transplanted for acute leukemia. Median follow-up was 1.6 years. Haploidentical allogeneic stem cell transplantation was more frequently performed for acute myeloid leukemia and in late stages than any other donor type. Non-relapse mortality at 100 days and one year for unrelated and haploidentical donors were similar, 19%-29% vs. 17%-28%, respectively. A significant better non-relapse mortality was observed for matched sibling donors (7%-15%; p < 0.001). Relapse rate was higher in haploidentical donors compared to matched sibling and unrelated donors (three year relapse rate 46%, 39%, 28%; respectively p < 0.001). Haploidentical donors resulted in lower three year progression-free survival and worse 3 year overall survival (32%; p < 0.001 and 42%; p < 0.001) compared with other donors (44% and 55% MSD, 40% and 42% UD, respectively). The incidence of grade II-IV acute graft-versus-host disease was higher in unrelated donors (51% unrelated, 35% haploidentical, 36% matched sibling; respectively; p = 0.001), with no difference in grades III-IV (p = 0.73) or in chronic graft-versus-host disease (p = 0.2) between groups. After multivariate analysis, haploidentical and unrelated donors remained negatively associated with non-relapse mortality (HR 1.95; 95% CI 1.10-3.20 and HR 2.70; 95% CI 1.63-4.46, respectively). Haploidentical donors were associated with a higher risk of relapse and worse overall survival. This analysis shows that haploidentical donors were associated with similar non-relpase mortality and higher relapse rates than unrelated donors. Better results in non-relapse mortality were observed for matched sibling donors.
Key words: hematopoietic stem cell transplantation, haploidentical transplantation, non-relapse mortality and donors
Dirección postal: José I. Trucco, Hospital Universitario Austral, Av. Presidente Perón 1500, 1629 Derqui, Provincia de Buenos Aires, Argentina
e-mail: jtrucco@cas.austral.edu.ar
Current knowledge
• Haploidentical transplantation is an alternative option for patients needing a transplant who lack a matched sibling donor or a suitable unrelated one. Previous retrospective studies showed similar or even lower non-relapse mortality and lower incidence or acute and chronic graft versus host disease with this type of donor, with similar progression-free and overall survival.
New knowledge
• This experience compares results in a large cohort of patients with malignant diseases, according to the type of stem cell donor used. In this experience, haploidentical transplantation carries similar non-relapse mortality, but lower overall survival than unrelated donor transplantation
Allogeneic stem cell transplantation (AlloSCT) is a potentially curative treatment for patients with hematological diseases. For those patients lacking a matched sibling donor (MSD), other options for AlloSCT include unrelated donors (UD) and haploidentical donors (HD). Searching for an UD is a time-consuming procedure, and striking differences are observed in the length of time employed with this strategy in many countries 1, 2. Haploidentical AlloSCT is an option when patients require urgent AlloSCT, since most of the patients account with a convenient HD.
The widespread use of post-transplant cyclophosphamide made HD AlloSCT a feasible and a more accessible option worldwide, especially in low-income countries, where UD AlloSCT is a more complicated therapeutic option in many aspects, including the cost of the procedure, the length of time of the search, and the cost of the procurement 3-4.
There are several studies from North America, Europe, and Asia comparing the results of HD with MSD and UD in different AlloSCT situations 5-9, however prospective clinical trials comparing AlloSCT outcomes according to the type of donor are needed. 10, since the majority of the reports are retrospective studies 11-15. A previous published report compared outcomes of acute lymphoblastic leukemia patients transplanted in Argentina 16. There are no publications describing the outcomes of AlloSCT in other hematological malignancies according to donor type in our region.
We conducted a multicenter retrospective analysis to compare the outcomes of AlloSCT according to these types of donors. Our main objective was to assess the non-relapse mortality (NRM) and overall survival (OS).
Materials and methods
We included consecutive adult patients (≥16 years old) who received an AlloSCT, between January 2012 and December 2016. Transplants were performed in 7 transplant units affiliated to GATMO-TC. The study was approved by local ethics committee according to Helsinki Declaration. All participating centers performed the three types of transplants. Patients who received a second AlloSCT or had a non-malignant disease were excluded. Data was obtained retrospectively from 570 medical records. Patients were followed longitudinally until death or last contact. Patients received a MSD, UD, or HD AlloSCT, depending on the center`s choice and donor availability.
UD donor category included matched 10/10 matched HLA antigens and 9/10 HLA-missmatched unrelated donors.
Stem cells graft sources included peripheral blood and bone marrow.
The variables analyzed were donor type; patient’s and donor’s age and sex; pre-transplant cytomegalovirus serological status; type of conditioning regime (myeloablative vs. reduced intensity); use of total body irradiation; type of immunosuppression; and stem cells source. Comorbidities were categorized using the hematopoietic cell transplantation – specific comorbidity index (HCT-CI) published by Sorror et al.17. Disease status was defined based on previous reports 18. Early stage disease included acute leukemia in first complete remission, myelodysplastic syndromes in first complete remission or with no previous treatment, and chronic myelogenous leukemia in first chronic phase, while other status was categorized as late stage disease.
Neutrophil and platelet engraftment were defined as achieving absolute neutrophil count ≥0.5 x 109/l for 2 consecutive days and ≥ 30 x 109/l platelets in two determinations, separated for at least 5 days, without transfusion. Fungal infections were defined as all confirmed fungal infection by positive culture and / or probable determined according to the physicians’ judgement. Acute graft-versus-host disease (aGVHD) and chronic graft-versus-host disease (cGVHD) were graded using Glucksberg and NIH classification 19, 20.
Our primary endpoints were non-relapse mortality (NRM), death from any cause without disease progression was considered an event, overall survival (OS), progression-free survival (PFS), and relapse. Secondary endpoints were engraftment rate, post-transplant cytomegalovirus reactivation, fungal infections, aGVHD and cGVHD incidence.
Statistical analysis was performed using SPSS, version 23.0 (SPSS Inc., Chicago, IL, USA), R, version 3.2 (R Foundation for Statistical Computing, Vienna, Austria. URL http://www.R-project.org/) and STATA, version 14.2 (Stata-Corp. 2015. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP). Overall Survival and PFS were calculated using the Kaplan-Meier method. Non-relapse mortality, relapse, and cGVHD were calculated using cumulative incidence analysis. Death or relapse was the competing risk for cGVHD. Relapse was the competing risk for NRM. Dichotomic variables were analyzed with the chi-square test. Multivariate analysis was constructed for transplantation outcomes using a Cox regression model. All the variables with a P-value of 0.2 or less were included in the analysis. Results were considered statistically significant if the P-value was < 0.05. Variables that were considered clinically relevant for specific outcomes were included in the multivariate analysis, even those in which the P-value was not < 0.2 (i.e. myeloablative conditioning when addressing NRM, acute myeloid leukemia for NRM, Rel, OS, PFS, and late stage for relapse).
Results
Median follow-up was 1.6 years. Main characteristics of the cohort are listed in Table 1. Patient´s mean age was 39 years (range 16-74 years) and donors’ mean age was 35 years (range 7-69 years). Almost sixty percent of the patients and the donors were males. Two hundred and forty patients (42%) received a MSD, 189 (33%) a UD (57% HLA-matched, 43% HLA-mismatched), and 141 (25%) a HD AlloSCT. Prevalent diseases were acute myeloid leukemia (AML) in 38% of the patients, acute lymphoid leukemia in 23%, myelodysplastic syndromes (MDS) in 15%, and lymphoproliferative diseases in 12%.
Two hundred and forty-one patients (42%) had a low HCTCI index, and 58% of the cohort was transplanted in the late stage of the disease. A myeloablative conditioning, mainly based on busulphan combinations, was used in 72% of the patients.
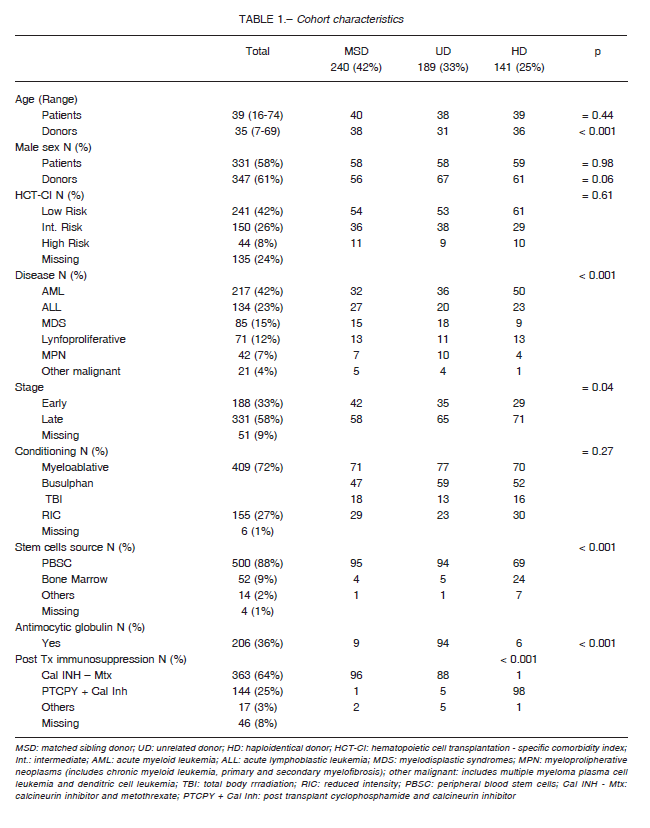
There were no differences in patient’s age, sex, pretransplant cytomegalovirus status, HCT-CI score, and type of conditioning regime between the three groups.
Unrelated donors were younger compared to MSD and HD (mean age 31y vs. 38y vs. 36y; respectively, p < 0.01).
Haploidentical AlloSCT were done more frequently in a late stage compared to MSD or a UD AlloSCT (71% vs. 58% vs. 65%; respectively p = 0.04). Acute myeloid leukemia was more frequent in HD AlloSCT than in MSD or UD AlloSCT (50% vs. 32% vs. 36%; respectively; ≤ 0.001), as it was for bone marrow graft source also (24% HD vs. 4% MSD vs. 5% UD, p < 0.001). Post- transplant cyclophosphamide-based immunosuppressive combination was the main choice in HD AlloSCT compared to the other groups (98% HD vs. 1% MSD vs. 5% UD, p < 0.001).
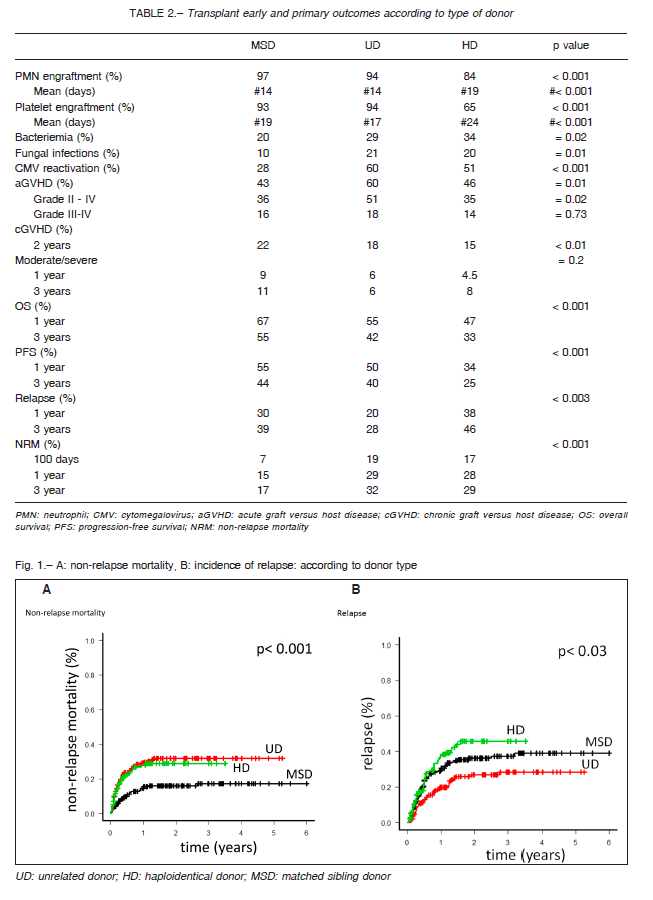
Neutrophil engraftment was slower in HD AlloSCT when compared to MSD and UD AlloSCT (mean 19 days vs. 14 days vs. 14 days, respectively; p < 0.001). A higher incidence of graft failure was also found in the HD group (16% in HD vs. 3% in MSD and 6% in UD; p < 0.001).
Similarly, platelet engraftment was significantly delayed in HD AlloSCT compared to the other groups (24 days in HD vs. 19 days in MSD vs. 17 days in UD; p < 0.001) (Table 2).
Cytomegalovirus reactivation occurred more frequently in HD and UD patients (60% and 51%, respectively vs. 28% MSD; p < 0.001) as well as post-transplant bacteremia (34% in HD vs. 29% in UD and 20% in MSD; p = 0.02).
Patients who received a HD or a UD graft developed posttransplant fungal infections more frequently (21% UD vs. 20% HD vs. 10% MSD; p = 0.01) (Table 2).
Unrelated AlloSCT recipients developed more frequently aGVHD (60% UD vs. 43% MSD vs. 46% HD; p =0.001), as well as grades II- IV (51% UD vs. 36% MSD vs. 35% HD; p = 0.02). There was no difference in incidence of severe forms of aGVHD (grades III-IV)
between groups (p = 0.73) (Table 2). We have not found any difference in the incidence of cGVHD between the three types of AlloSCT (Table 2).
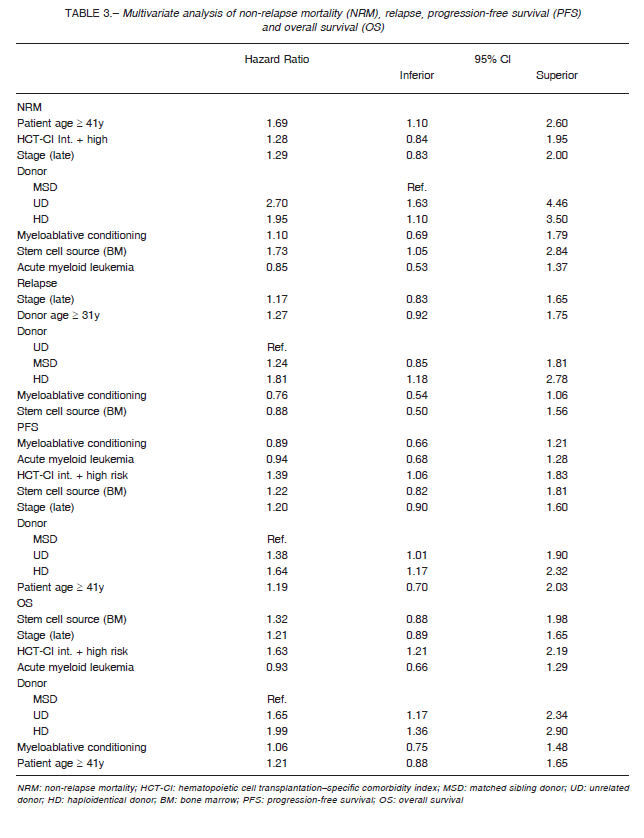
Early mortality, expressed as NRM at 100 days, was 7% in MSD, 19% in UD, and 17% in HD. Non-relapse mortality at 1 and 3 years (1-3 y) was 15-17%, 29-32%, and 28-29%, respectively (p < 0.001) (Fig. 1A). After the multivariate analysis (expressed as Hazard Ratios with 95% confidence intervals), HD and UD AlloSCT were independently associated with a higher NRM (HR: 1.95, 95% CI 1.10-3.50 for HD; HR 2.70, 95% CI 1.63-4.46 for UD) compared to MSD recipients. Similarly, older age (age ≥ 41 years) or bone marrow as stem cell graft source remained significantly associated with this event (Table 3).
There were no differences in NRM and OS between matched and mismatched UD donors; therefore, we analyzed them as a whole category (data not shown).
To address the missing data and looking for a reduction in bias interference, a multivariate analysis, including myeloablative conditioning and a second multivariate analysis excluding HCT-CI, were conducted. No differences were found in these results (data not shown).
Relapse rate (1-3 y) was higher in HD and MSD AlloSCT compared to UD AlloSCT (38-46% vs. 20-39% vs. 20-28%, respectively; p < 0.003) (Fig. 1B). When adjusted for other variables, HD AlloSCT (HR 1.81, 95% CI 1.18-2.78) was the only independent factor remaining associated with almost 2-fold increase risk of relapse (Table 3).
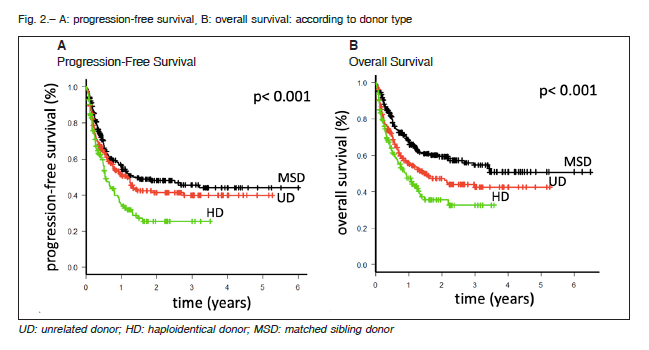
Haploidentical AlloSCT resulted in lower PFS (1-3 y 34-25% HD vs. 55-44% MSD vs. 50-40% UD; p < 0.0001) (Fig. 2A) and OS (1-3 y 47-33% HD vs. 67-55% MSD vs. 55-42% UD; p < 0.001) (Fig. 2B) when compared to the other transplant groups. After the multivariate analysis, HD AlloSCT remained significantly associated with worst OS (HR: 1.99, 95% CI 1.36-2.90) and PFS (HR 1.64, 95% CI 1.17-2.32). Another factor independently associated with OS and PFS was an intermediate to high HCT-CI risk (Table 3).
Discussion
In this retrospective cohort analysis, NRM after HD and UD AlloSCT was similar; with lower OS and PFS for HD AlloSCT due to a higher relapse rate. Acute GVHD II–IV was higher than expected in the HD transplant setting.
Although some publications 14, 15, 17 encourage the choice of HD in the absence of a MSD, in our experience there were some benefits for those patients who received an UD transplant, as other studies have previously shown 26.
We found that both the incidence of the graft failure and the neutrophil recovery time, were higher in patients who received a HD AlloSCT in comparison to the other groups of patients. Similar results have been published by other authors 8, 10 , raising the hypothesis that post-transplant cyclophosphamide could be the main cause for this delayed bone marrow recovery. Recently, Rashidi et al.11 compared 83 newly diagnosed AML patients who received an AlloSCT, either HD, MSD, or UD. They uniformly used post-transplant cyclophosphamide as primary GVHD prophylaxis in the three types of transplants. Both neutrophil and platelet recovery times were longer in the HD AlloSCT group. This fact raises the possibility that the engraftment delay may be mainly due to HLA disparity rather than to the use of post-transplant cyclophosphamide, as it was previously considered.
Although the results vary across different studies, we observed a higher incidence of aGVHD in HD AlloSCT, compared to previously published results 21-23. This was observed in grade II-IV disease, without any differences in grade III-IV aGVHD. This is probably due to the fact that HD graft source was peripheral blood stem cell (PBSC) in around 70% of the cases. Higher risk of aGVHD II-IV in the HD setting secondary to the use of PBSC as graft source, has also been reported both by Sanz et al.24 and Ruggeri et al.25 (HR 1,93; p<0.001 and HR 2.1; p<0.001). We found a higher aGVHD incidence in patients who received a UD AlloSCT compared to what has been published in previous reports 10, 15. We understand that this increment can be explained by the inclusion of a considerable proportion of HLA-missmatched UD. Interestingly, the extended use of peripheral blood as a source for stem cells did not increase the incidence of cGVHD in the HD AlloSCT cohort, as it would have been expected 12.
In our cohort, UD and HD AlloSCT had similar early as well as long term NRM, raising the question about transplant-related toxicity with these types of donors.
Regarding this issue, data published is controversial.
Bashey et al.9 reported the outcomes of 271 patients who received an AlloSCT in a single American center for hematological malignancies. No differences in NRM were found between groups (1y NRM was 10% for UD in comparison to 4% for HD AlloSCT), although it was considerably lower when compared to our cohort results (one year NRM 25% vs. 26%, respectively). In another study carried out by the European Group for Blood and Marrow Transplantation (EBMT). Piemontese et al.13 compared the results from HD and UD AlloSCT in a cohort of 3568 patients with acute leukemia in first or second remission.
The results published are similar to ours (three year NRM of 29% for the HD group and of 21% for the UD group).
After a multivariate analysis, in our experience, there was a 2-fold increase in NRM risk for the HD AlloSCT and more than 2.5-fold increase for the UD AlloSCT. In a multicenter cohort, Shouval et al.26 reported outcomes on the largest population published, with 106 188 patients transplanted from allogeneic donors for multiple malignancies.
They showed an improvement in NRM across the time, especially for HD AlloSCT, with a reduction from 59.3% after 3 years, when the patient was transplanted between 2001 and 2005, to 27.3% after 3 years, when the patient was transplanted between 2011 and 2015.
Despite this, when compared with UD, and stratified by disease risk, HD AllosSCT resulted in a higher risk for NRM in all risk stratifications. Our cohort included adult patients with multiple hematological malignancies and most of them arrived to transplant in a late stage of the disease.
In our experience, relapse was significantly higher in the HD AlloSCT group when compared primarily with the UD AlloSCT group. These results are similar to those reported by Ciurea et al.27. In our cohort, most of the patients from the HD AlloSCT group were at ‘high risk’ for relapse, as most of them were transplanted at late stage. Evidence in the literature is controversial, with other groups reporting similar relapse rates between diverse donors 22.
Post-transplant cyclophosphamide could play a role in higher relapse rate. Some published data contradicts this hypothesis 12, 24. The difference in the graft source may be responsible for the higher relapse rate. Recently, a retrospective study published by Bashey et al.15 found a higher risk of relapse in patients with AML and MDS who were transplanted with HD bone marrow grafts in comparison to those who received PBSC grafts (HR 1.75; p = 0.002). This outcome was not explained by a lower incidence of graft versus leukemia effect in that group (HR 2.13; p = 0.01for relapse), however it could be due to the higher use of reduced intensity conditioning. A recent systematic review has been published focusing on the comparison of outcomes in HD alloSCT depending on the type of graft source used 28. No differences in relapse rate were found with any of these grafts (pooled OR: 0.532 95%CI 0.18-1.56).
Our study has certain limitations. The retrospective design may have contributed to missing data or loss to follow up data, which resulted in a bias in the primary endpoints results. In Argentina, HD alloSCT have become frequently used since 2014. The short period of time considered for the study of this cohort did not allow us to perform analysis by periods. There could be a bias on the time elapsed for selecting these patients. Haploidentical alloSCT has formerly been used as a salvage therapy for heavily pretreated or very high-risk patients, with a shorter period to proceed to the transplant compared to those receiving a UD transplant, who had longer waiting periods due to the length of the searching process. These facts could
explain the worse outcomes for freedom from progression in the HD group of our population. In the largest cohort of patients comparing these three sources of transplants, Shouval et al 26 from EBMT showed worse outcomes for the HD group, with a clear ‘learning curve’ effect over the time.
These results are according to our experience. It is probable that this effect could be demonstrated in the future for HD AlloSCT, especially for NRM. On the other hand, there was heterogeneity in the conditioning regimens used amid transplant centers, and this could have contributed to the diverse NRM between groups.
Our study has the value of a comparison of the three type of donors for AlloSCT in a large cohort with malignant diseases in Argentina.
Although HD alloSCT is a feasible therapeutic option in our region, some concerns on toxicity have arisen, in coincidence with other experiences 26. In this report, HD alloSCT is associated with higher relapse rate and similar NRM than UD alloSCT, as well as with worse outcomes than MSD alloSCT. Larger prospective trials should be conducted to try to answer this point. While HD AlloSCT allows for a rapid source for transplantation in high-risk patients, UD AlloSCT is still a valid option in our region and efforts should be focused in shortening the donor searching time in order to improve results with this source of stem cells.
Acknowledgements: We thank the physicians from the transplant centers who made possible the collection of clinical data
Conflict of interest: None to declare
References
1. Gragert L, Eapen M, Williams E, et al. HLA match likelihoods for hematopoietic stem-cell grafts in the U.S. registry. N Engl J Med 2014; 371: 339-48.
2. Rosenmayr A, Pointner-Prager M, Mitterschiffthaler A, et al. What are a patient’s current chances of finding a matched unrelated donor. Twenty years central search experience in a small country. Bone Marrow Transplant 2012; 47: 172-80.
3. Rodríguez-Arbolí E, Márquez-Malaver FJ, Rodríguez-Torres N, et al. Allocation to matched related or unrelated donor results in similar clinical outcomes without increased risk of failure to proceed to transplant among patients with acute myeloid leukemia: a retrospective analysis from the time of transplant approval. Biol Blood Marrow Transplant 2019; 25: 183-90.
4. Ciurea SO, Bittencourt MCB, Milton DR, et al. Is a matched unrelated donor search needed for all allogeneic transplant candidates? Blood Adv 2018; 2: 2254-61.
5. Ruggeri A, Battipaglia G, Labopin M, et al. Unrelated donor versus matched sibling donor in adults with acute myeloid leukemia in first relapse: an ALWP-EBMT study. J Hematol Oncol 2016; 9: 89
6. Zhang MJ, Davies SM, Camitta BM, Logan B, Tiedemann K, Eapen M. Comparison of outcomes after HLA-matched sibling and unrelated donor transplantation for children with high-risk acute lymphoblastic leukemia. Biol Blood Marrow Transplant 2012; 18: 1204-10.
7. How J, Slade M, Vu K, et al. T cell-replete peripheral blood haploidentical hematopoietic cell transplantation with post-transplantation cyclophosphamide results in outcomes similar to transplantation from traditionally matched donors in active disease acute myeloid leukemia. Biol Blood Marrow Transplant 2017; 23: 648-53.
8. Raiola AM, Dominietto A, di Grazia C, et al. Unmanipulated haploidentical transplants compared with other alternative donors and matched sibling grafts. Biol Blood Marrow Transplant 2014; 20: 1573-9.
9. Bashey A, Zhang X, Sizemore CA, et al. T-cell-replete HLA-haploidentical hematopoietic transplantation for hematologic malignancies using post-transplantation cyclophosphamide results in outcomes equivalent to those of contemporaneous HLA-matched related and unrelated donor transplantation. J Clin Oncol 2013; 31: 1310-6.
10. Wang Y, Liu QF, Xu LP, et al. Haploidentical vs identicalsibling transplant for AML in remission: a multicenter, prospective study. Blood 2015; 125: 3956-62.
11. Rashidi A, Slade M, DiPersio JF, Westervelt P, Vij R, Romee R. Post-transplant high-dose cyclophosphamide after HLA-matched vs haploidentical hematopoietic cell transplantation for AML. Bone Marrow Transplant 2016; 51: 1561-4.
12. Bradstock K, Bilmon I, Kwan J, et al. Influence of stem cell source on outcomes of allogeneic reduced-intensity conditioning therapy transplants using haploidentical related donors. Biol Blood Marrow Transplant 2015; 21: 1641-5.
13. Piemontese S, Ciceri F, Labopin M, et al. A comparison between allogeneic stem cell transplantation from unmanipulated haploidentical and unrelated donors in acute leukemia. J Hematol Oncol 2017; 10: 1-8.
1 4. Solomon SR, Sizemore CA, Sanacore M, et al. Total body irradiation-based myeloablative haploidentical stem cell transplantation is a safe and effective alternative to unrelated donor transplantation in patients without matched sibling donors. Biol Blood Marrow Transplant 2015; 21: 1299-307.
15. Bashey A, Zhang MJ, McCurdy SR, et al. Mobilized peripheral blood stem cells versus unstimulated bone marrow as a graft source for T-cell-replete haploidentical donor transplantation using post-transplant cyclophosphamide. J Clin Oncol 2017; 35: 3002-9.
16. Basquiera A, Berro M, Yantorno S, et al. Haploidentical transplant in adult patients with acute lymphoblastic leukemia in Argentina: a comparison with matched related and unrelated donors. Bone Marrow Transplant 2020; 55: 400-8.
17. Sorror ML, Maris MB, Storb R, et al. Hematopoietic cell transplantation (HCT)-specific comorbidity index: a new tool for risk assessment before allogeneic HCT. Blood 2005; 106: 2912-9.
18. Barrett AJ, Battiwalla M. Relapse after allogeneic stem cell transplantation. Expert Rev Hematol 2010; 3: 429-41.
19. Glucksberg H, Storb R, Fefer A, et al. Clinical manifestations of graft-versus-host disease in human recipients of marrow from hl-a-matched sibling donors. Transplantation 1974; 18: 295-304.
20. Jagasia MH, Greinix HT, Arora M, et al. National Institutes of Health consensus development project on criteria for clinical trials in chronic graft-versus-host disease: I. The 2014 diagnosis and staging working group report. Biol Blood Marrow Transplant 2015; 21: 389-401.e1.
21. Bashey A, Solomon SR. T-cell replete haploidentical donor transplantation using post-transplant CY: An emerging standard-of-care option for patients who lack an HLA-identical sibling donor. Bone Marrow Transplantation 2014; 49: 999-1008.
22. Shaw BE. Related haploidentical donors are a better choice than matched unrelated donors: counterpoint. Blood Adv 2017; 1: 401-6.
23. Lee CJ, Savani BN, Mohty M, et al. Haploidentical hematopoietic cell transplantation for adult acute myeloid leukemia: a position statement from the acute leukemia working party of the European Society for Blood and Marrow Transplantation. Haematologica 2017; 102: 1810-22.
24. Sanz MA, Iacoboni G, Montesinos P, Venditti A. Emerging strategies for the treatment of older patients with acute myeloid leukemia. Ann Hematol 2016; 95: 1583-93.
25. Ruggeri A, Labopin M, Bacigalupo A, et al. Bone marrow versus mobilized peripheral blood stem cells in haploidentical transplants using posttransplantation cyclophosphamide. Cancer 2018; 124: 1428-37.
26. Shouval R, Fein JA, Labopin M, et al. Outcomes of allogeneic haematopoietic stem cell transplantation from HLA-matched and alternative donors: a European Society for Blood and Marrow Transplantation registry retrospective analysis. Lancet Haematol 2019; 3026: 1-12.
27. Ciurea SO, Zhang MJ, Bacigalupo AA, et al. Haploidentical transplant with posttransplant cyclophosphamide vs matched unrelated donor transplant for acute myeloid leukemia. Blood 2015; 126: 1033-40.
28. Xiaotong Y, Liping L, Zhenwei X, et al. Bone marrow versus peripheral blood as a graft source for haploidentical donor transplantation in adults using post-transplant cyclophosphamidea systematic review and meta – analysis. Critical Reviews in Oncology / Hematology 2019; 133: 120-8.
